New Spatial Maps of the Intestine Show Cell-Level Details
ACS grantee contributed his cellular spatial map of the large and small intestine to a larger project, the Human BioMolecular Atlas Program (HuBMAP).
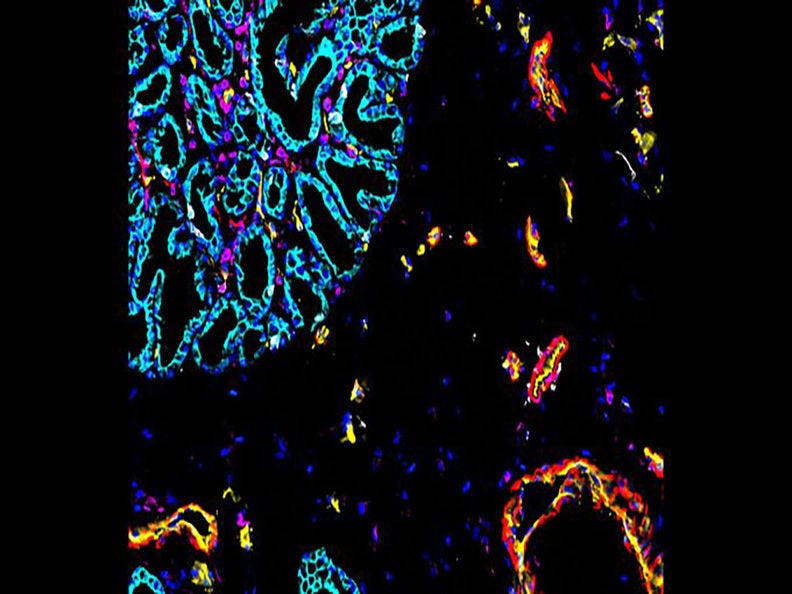
This is a CODEX fluorescence image of the intestines. This new type of imaging stains cells different colors. Courtesy: John Hickey, PhD, Duke University
The Challenge
Back in the old days, before almost every phone and car had GPS (Global Positioning System) technology, people had to unfold an unwieldy paper map to take a road trip. Some called AAA and asked for a TripTik to their destination. An upgrade from a regular map, TripTiks included several neatly bound maps, highlighted in multiple colors with sticky notes to make navigation easier to follow. More detailed, yes, but still unwieldy. Plus, they couldn’t predict closed roads or a wreck ahead.
When it comes to understanding the position of cells in organs and how they work to form tissues—or malfunction in diseases like cancer—the effectiveness of today’s technology is somewhere between a big, folded map and a TripTik. Scientists long for something like GPS for the body—a sophisticated map that gives the precise location of a cell and information about its neighborhood.
That’s why 3,000 scientists in nearly 100 countries are working with tissues from 10,000 donors to construct the Human Cell Atlas (HCA) and a component of it known as the BioMolecular Atlas Program (HuBMAP). The program’s goal is to construct comprehensive 3-dimensional, spatial maps that feature a range of molecules such as RNA, proteins, and metabolites in healthy human organs. This atlas will be at single-cell resolution, which means researchers can study RNA and other molecules in different cells within the same tissue (aka the cells’ neighborhood).
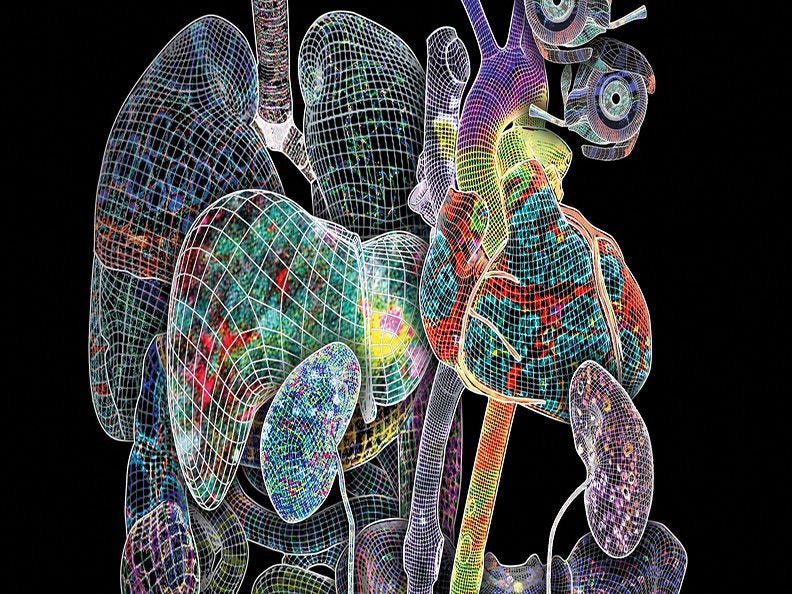
This is the cover image from the issue of Nature that featured 13 scientific papers about HuBMAP research, including Hickey’s about the spatial map of the intestine. Credit: Heidi Schlehlein, Indiana University, and the HuBMAP Consortium
We’ve learned that diverse types of cells are common to all portions of the intestines and that some cell types aggregate in certain regions. It’s thought that the localization of individual cell types drives distinct functions.
What we don’t know yet is how these localized cell types vary in different regions of the intestine. We don’t always know why cells coordinate to create healthy tissue, or what happens when diseases start.
Learn More About It
Want a more basic understanding of precision therapy, cell therapy, and single-cell resolution?
The Research
Using modern technologies to get information about the location of cells and how that location affects their function is part of the mission for Dr. John Hickey’s lab, which opened in January 2024. He’s an American Cancer Society (ACS) grantee with special funding from Marianne Kipper and the Roaring Fork Valley Research Circle. He’s now at Duke University in Durham, North Carolina and is the first biomedical engineering researcher specializing in spatial biology at Duke.
Hickey recently published a study in Nature describing discoveries he contributed to while he was a postdoctoral fellow at Stanford under the mentorship of Garry P. Nolan, PhD. The researchers mapped the small and large intestines at the level of single cells. They analyzed 8 sections of the intestine from 9 people, ages 28 to 78.
The study supported findings from previous research about spatial maps of cells and proteins that used single-cell RNA technologies like this team did. The team also expanded the field of cell mapping by completing the first in-depth spatial study of single cells in the intestine.
Why focus on mapping the intestines?
The intestine is the largest immune organ in the body. So, evaluating the location and interactions of the immune cells in the gut is critical for understanding immunotherapies for cancer, as well as for the design of oral vaccines, interactions that regulate the gut microbiota, food allergies, and wound repair.”
John Hickey, PhD
Duke University
Former American Cancer Society Postdoctoral Fellow Grantee

Part of their technique involved using a new imaging platform called Co-Detection by Indexing (CODEX). CODEX attaches color-coded antibodies to the proteins on the surface of cells creating a colorful—and informative—image of the variety of cells in tissue. Then the researchers deploy machine learning algorithms and other computational tools to identify the types of cells in the tissue sample and to measure how close they are to each other.
“We showed the extensive cellular complexity of the intestine, revealing that different regions of healthy intestines have different cell compositions, that cells are organized into different cellular ‘neighborhoods’ in the tissue, and that those neighborhoods form ‘communities’ defined by distinct areas of epithelial and immune cells,” says Hickey. “We can see where and how cell types are grouped and study how they interact.”
The researchers even identified several unique cellular neighborhoods within the intestine.
“Together, these data provide a detailed atlas that can serve as a valuable reference for future studies of the intestine,” the authors wrote.
Researchers will certainly have the chance to use his data as Hickey’s cellular map of the intestines is described in a recent article that overviews the spatial maps of organs being collected as part of the HuBMAP. Data from the HuBMAP is available to scientists online.
With the cellular map of the intestine in hand, Dr. Hickey’s new lab team has their own set of questions to answer to further the knowledge about the cell's capacity and function. They aim to continue their investigation with the hope of developing new biomaterials and cellular therapies to correct and control the function of the cell and the structure of tissues.
- Are there cells that are the primary drivers of tissue organization?
- What is a cell’s capacity to rearrange or maintain its microenvironment?
- How can we control a cell's capacity to rearrange or maintain its microenvironment?
- Can we use this information to reverse cellular disorders we observe in diseased tissue like cancer?
Why It Matters
“It's really hard for researchers like me to get healthy tissue to compare to diseased tissue (like cancer) for scientific studies," Hickey says. “There's plenty of diseased tissue to study because surgeons remove it for biopsies or treatment. This atlas will be foundational as a resource for scientists who want to see if and how cell geography in healthy tissue compares with diseased tissue,” he explains.
Hickey’s cellular spatial map of the intestine and the other maps in the HuBMAP atlas can also be used to expand precision therapy in general, and to expand subsets of that therapy, such as tissue- and cell-specific drug targeting.
Cell therapy is a quickly expanding area, and it could be accelerated by the development and rapid commercialization of analytical tools that can decode molecular contents at the single-cell level.
The discovery of new types of cell therapy could help many health problems including cancer, as well as disorders in the nervous system and heart, type 2 diabetes, diseases of bones and joints, genetic disorders, and wounds of the skin.
Featured Term: Cell therapy
The prevention or treatment of certain diseases using specifically selected cells rather than chemical compounds used in chemotherapy and some targeted therapies. The cells can come from a donor or the patient, multiplied, genetically or pharmacologically altered in a lab, and returned to a patient, often by IV infusion.
Bone marrow and stem cell transplants are the most frequently used cell therapy. They’re used to treat cancers in the blood. Another more recently discovered cell therapy is CAR (chimeric antigen receptor) T-cell therapy, which is being used to treat certain blood cancers. Scientists are studying how to use cell therapy in solid tumors. (See Stem Cell or Bone Marrow Transplant and CAR T-cell Therapy and Its Side Effects)
For more definitions, go to the Glossary for Nonscientists.
Donations from people like you make this research possible. Thank you for helping rid the world of cancer.
- Helpful resources
- For researchers


