Your gift is 100% tax deductible
Insurance Links Cancer Screening Rates with Unemployment
ACS researchers reveal the need to protect cancer screening rates when unemployment is high, such as during the COVID-19 pandemic.
The Challenge
During the COVID-19 pandemic unemployment rates in the US rose to levels that haven’t been so high since the Great Depression. Job loss may lead to both reductions in income and access to employer-based health insurance coverage. And not having health insurance is a barrier to receiving preventive care, including cancer screening.
In fact, people without health insurance are half as likely to be up to date with recommended screening for breast, cervical, and colorectal cancer.
We need information about the extent to which health insurance coverage explains the relationship between unemployment and cancer screening to inform the economic impacts of the COVID-19 pandemic as well as future adverse events on cancer screening.
The Research
A team of ACS researchers in Surveillance and Health Equity Science, led by Stacy Fedewa, MPH, PhD, the previous senior principal scientist of risk factors and screening surveillance research at the ACS, examined how often people received cancer screening according to job status.
Their published results included these findings:
- Nonelderly people who were unemployed were 10% to 30% less likely to be up to date with recommended screening, and the unemployment gap in screening was fully explained by lack of health insurance.
- Adults who were unemployed were 4 times more likely to be uninsured compared to employed adults.
Cancer Screening Rates According to Employment Status
We found that health insurance coverage fully accounted for fewer cancer screenings among unemployed adults in the United States. That discovery is particularly noteworthy because it’s potentially modifiable. The US could ease some economic distress from the COVID-19 pandemic by developing and approving comprehensive health policies that ensure health insurance coverage and access to preventive care while people are unemployed. Such policies are required to protect cancer screening for future economic downturns too. A finding from another study that policy makers may find worth considering for the future is that increases in unemployment only increased cancer death rates in countries that don’t have universal health coverage. Universal health coverage seems to erase the links between employment and cancer screening rates as well as between employment and cancer death rates.”
Stacey Fedewa, MPH, PhD
Surveillance, Prevention, & Health Services Research
American Cancer Society

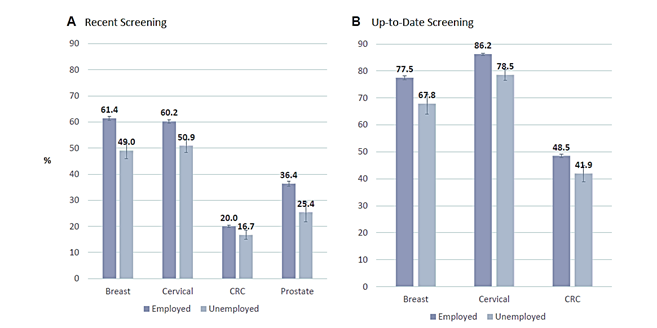
Graph A compares the percentage of people who were employed vs unemployed who were screened recently (in the last year) for breast, cervical, CRC (colorectal), or prostate cancer. Graph B compares the same groups for people who were up to date with screening recommendations. It doesn’t show prostate cancer because the screening guideline calls for men to discuss whether or not to get screened for prostate cancer with their doctor.
- Being unemployed seemed to be similarly harmful to cancer screening across racial/ethnic groups, although Black adults were 70% more likely to be unemployed than White adults and Hispanic adults were 50% more likely.
- Being unemployed at any time may hinder recent and longer term screening practices. This is concerning because not getting screened is the first step on a path of less effective treatment choices, which includes raising the potential for more treatment side effects and increasing the risk of dying from cancer.
The ACS research team estimated that the number of adults eligible for screening who were unemployed doubled between 2018 before the pandemic and 2020 during it.
The authors said further research is needed on the link between cancer care and state-level unemployment benefit generosity, as well as Medicaid expansion, one of the provisions to expand health insurance coverage in the Affordable Care Act (ACA). They also emphasized that these findings highlight the importance of and need for comprehensive health policies that ensure health insurance coverage and access to health care while people are unemployed.
Findings Specific to Colorectal Cancer Screening. Those who were uninsured and employed had the lowest CRC screening even when compared to those uninsured and unemployed. People who are working and who don’t have health insurance may have additional barriers to cancer screening besides paying for it. For instance, getting a colonoscopy often requires paid sick leave because this test requires a full day off work and a chaperone to get home after the procedure.
Of the cancer screenings analyzed, the researchers found that decreases in colorectal cancer and cervical cancer based on unemployment could be eliminated based on a higher household income.
Why It Matters
Not being up-to-date with screening increases a person’s risk of being diagnosed with late-stage breast cancer, cervical cancer, and colorectal cancer. Cancers diagnosed at a later stage are generally more complicated to treat and may have poorer outcomes compared with cancers found at an early stage.
Within large health systems, more than half of late-stage breast cancers have been attributed to not being screened with mammography and 75% of deaths from colorectal cancer have been attributed to not being up to date with cancer screening.
For colorectal cancer screening, in particular, screening with colonoscopy helps prevent many cases of colorectal cancer because it allows doctors to remove precancerous polyps. Screening with stool tests, sigmoidoscopy, and/or colonoscopy can all help find colorectal cancer early, when it less complicated to treat.
Expanding and ensuring health insurance coverage after job loss may mitigate the COVID‐19 pandemic's economic impact, as well as the impact of future adverse economic events, on cancer screening.
- Related resources
- For researchers



