Cancer-related Mental Distress
Cancer doesn’t just affect your physical health. For my people it also causes anxiety, depression, PTSD, and other types of mental distress. Cancer-related mental distress can happen at any time, even weeks or months after treatment ends.
There are steps you can take to manage your distress.
- What is cancer-related mental distress?
- Types of mental distress
- What causes cancer-related mental distress?
- When does it usually start?
- What are the symptoms of mental distress?
- Who is most at risk?
- Doesn't everyone feel distressed when they have cancer?
- How mental distress affects cancer treatment and side effects
- Screening
- Talking to your health care team
- Treatments
- What caregivers, friends, and family can do
- Find more support
What is cancer-related mental distress?
Cancer-related mental distress is a general term for the many feelings and emotions that come with having cancer.
Mental distress is not the same as having problems or stressors in your life. Stress isn’t always negative. It can motivate and focus us. But sometimes, the problems and stressors in your life (like cancer) affect your thoughts and feelings so much that it becomes hard to cope.
People describe mental distress in many ways. If you have mental distress, you might feel:
- Sad or depressed
- Anxious
- Angry
- Hopeless
- Alone or isolated
- Helpless, or like you have no control
- Unsure of your purpose or meaning in life
- Numb, or nothing at all
- Exhausted
Mental distress can make it hard to function. You might have trouble scheduling appointments, making decisions, or taking medicines that are important for your cancer treatment and survivorship.
You might also struggle with activities not related to your cancer, like doing housework, talking to friends, or taking care of yourself.
Types of mental distress
Some of the most common types of cancer-related mental distress are:
- Anxiety
- Depression
- Stress disorders (post-traumatic stress, PTSD, and acute stress disorder)
It’s common to have more than one type of mental distress during your cancer treatment and survivorship journey. You might experience these together, or at different times.
What causes cancer-related mental distress?
There are many ways cancer and cancer survivorship can cause mental distress. This includes:
- Worries about the future
- Increased health needs (more appointments, doctors, and medicines)
- Long-term and late side effects
- Concerns about family and relationships
- Insecurity around body image and intimacy
- Fertility concerns and sexual dysfunction
- Money and/or health insurance stress
- Fear of cancer recurrence (FCR)
- Survivor’s guilt
When does it usually start?
Distress can happen at any time. It can also come and go during cancer treatment and survivorship. But there are certain times that often bring feelings of distress.
- When you are first diagnosed
- Before you start a new type of treatment
- When dealing with side effects of cancer treatment
- After treatment ends (survivorship)
Cancer survivors are at greater risk of developing a mental health disorder after treatment ends. This is often due to fear of recurrence, fewer check-up appointments, and less support.
This might take you by surprise. Cancer survivors often say they are surprised at the mental distress they feel after treatment ends.
What are the symptoms of mental distress?
Many of the symptoms of mental distress are hidden, so it can be hard to know if a person is struggling. They might seem “fine” on the outside. You might not even realize when you are distressed.
You might feel:
- Guilt, shame, or blame related to your cancer
- Sad, hopeless, or depressed most of the time
- More irritable or angry than usual
- Numb or disconnected from yourself (dissociation)
Other common symptoms are:
- A lack of interest in doing things or seeing people (or self-isolating)
- Avoiding certain people, places, or things
- Nightmares, flashbacks, or intrusive thoughts
- Hypervigilance (extreme caution, attention, or sensitivity to something)
- Wishing or hoping for death
- Having specific thoughts or plans to kill oneself (active suicidal ideation)
988 Suicide & Crisis Lifeline
988 Suicide & Crisis Lifeline provides 24/7, free and confidential support via phone or chat for people in distress, resources for you or your loved ones, and best practices for professionals. Includes information on finding your local crisis center.
Phone: 988
- Interpretation for more than 240 languages
- ASL Videophone for people who are deaf or hard of hearing
Text: 988 (English and Spanish only)
Website: http://suicidepreventionlifeline.org
To get immediate help, you can also go to the emergency department or call 911.
Who is most at risk?
Some people are more likely to struggle with severe mental distress that prevents them from living their lives.
You might be at greater risk for developing cancer-related mental distress if you have:
- A history of a mental health condition before cancer
- A history of substance use disorder
- A history of abuse or trauma
- Other health conditions
Where you live, grow, work, learn, and play also affects your mental health.
You are more likely to be affected by mental distress if you struggle with basic needs like stable housing, transportation, social support, and access to affordable and nutritious food.
These non-medical needs (called social determinants of health, or SDOH) can make a big difference to your physical and mental health.
Some of these things can’t easily be changed. But there are ways you can get help during your cancer treatment.
Find resources to help you during your cancer treatment:
Doesn't everyone feel distressed when they have cancer?
It’s common to feel some amount of distress when you or a loved one has cancer. You might feel overwhelmed and anxious about all of the unknowns. It might even feel like your life is out of control. This is normal.
A lot of things can go through your mind during this time. You might wonder:
- Why me?
- Did I do something to cause my cancer?
- What will the future look like for me and my loved ones?
It’s also common to feel anxious or worried about:
- Cancer treatments and the possible side effects
- Money, working, insurance, paying bills, or supporting your family
- Helping your friends, family, and caregivers cope
- Spiritual or existential concerns
These are all expected responses to a very distressful and often traumatic event. Just like other side effects, these feelings of distress can usually be managed.
Take steps early to manage your distress
If you feel distressed, don’t wait. It’s important to take steps early. Don’t wait until you reach a level of severe distress before you look for ways to cope. It’s much easier (and more effective) to start managing your distress before you get overwhelmed.
Do what you can, when you can
It’s not always possible to get help early. That’s okay, too. You might not even be aware of your distress until after it becomes unbearable. The most important thing is to get help as soon as you notice it.
Try to do what you can, when you can.
How mental distress affects cancer treatment and side effects
Managing your mental distress is also an important part of managing your cancer care.
Mental distress can make some of the physical side effects of cancer and cancer treatment worse. This is especially true of fatigue, nausea and vomiting, sleep problems, and pain.
Studies also show that people with unmanaged mental health conditions are more likely to have worse cancer-related outcomes, including survival and quality of life.
If it seems like you might have severe distress, your doctor or cancer care team may want to rule out other health problems that could be making it worse. They might also offer resources or a referral to a specialist.
Screening
Many experts recommend screening everyone with cancer for anxiety and depression. If your health care team asks you about your mental health, share how you’re really feeling.
They might ask questions to learn more about:
- Thoughts or feelings you are having
- How often you have those feelings, and how intense they are
- Physical symptoms that might be connected to your anxiety
- How these symptoms affect your day-to-day life
- If you’re thinking of hurting yourself or anyone else
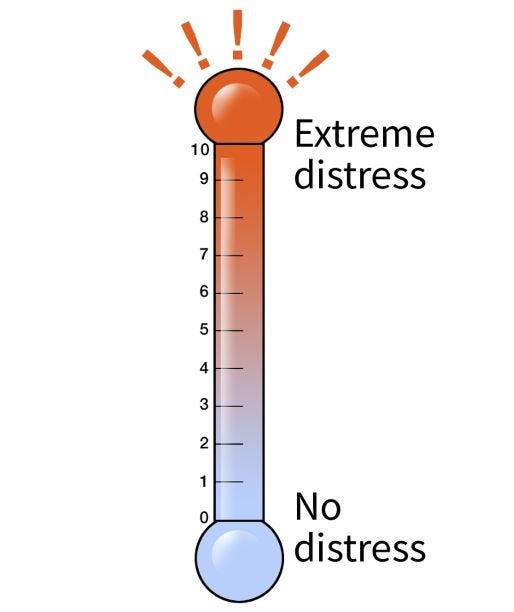
Measuring distress on a scale
Some cancer care teams measure distress in the same way, using a 0 to 10 scale. A common tool used by many providers is the distress thermometer.
The distress thermometer
If your care team uses the distress thermometer, you will be asked to circle the number (0-10) that best describes how much distress you had during the past week, including the present day.
Talking to your health care team
It can be hard to talk about mental health and distress. It might help to write down some of the symptoms you’re having or questions you want to ask. Here are a few ideas:
- Can my symptoms be managed?
- What types of treatments do you recommend?
- Would medication help?
- Can I talk with a therapist or specialist about my symptoms?
- Can you recommend a support group for me?
Treatments
Managing mental distress is very personal and individualized. It depends on each person’s specific situation, lifestyle, and needs.
Treatment might include talk therapy, medication, or a combination of both. Sometimes other specialized treatments or integrative therapies are used along with standard treatment. The goal is to improve your symptoms, reduce your suffering, and improve quality of life.
Examples of therapies that might be used to treat cancer-related mental distress are:
- Psychotherapy (talk therapy)
- Support or peer groups
- Education and resources for lifestyle habits (nutrition, good sleep, physical activity)
- Mindfulness-based activities (meditation, progressive muscle relaxation, yoga, breathwork, imagery)
- Creative therapies or activities (art, writing, dance, music)
- Medicines for specific mental health conditions like anxiety or depression
Learn more in Coping with Distress.
What caregivers, friends, and family can do
Find more support
- Written by
- References

Developed by the American Cancer Society medical and editorial content team with medical review and contribution by the American Society of Clinical Oncology (ASCO).
Aburizik A, Raque TL, Spitz N, Mott SL, McEnroe A, Kivlighan M. Responding to distress in cancer care: increasing access to psycho oncology services through integrated collaborative care. Psychooncology. 2023; 32(11): 1675-1683. https://doi.org/10.1002/pon.6217
Borenstein J. Stigma, prejudice, and discrimination against people with mental illness. American Psychiatric Association. August 2020. Accessed December 15, 2023. https://www.psychiatry.org/patients-families/stigma-and-discrimination
Cancer.net. Depression. Updated October 2022. Accessed May 24, 2024.
Chen WC, Boreta L, Braunstein SE, et al. Association of mental health diagnosis with race and all-cause mortality after a cancer diagnosis: Large-scale analysis of electronic health record data. Cancer. 2022. https://doi.org/10.1002/cncr.33903
National Comprehensive Cancer Network. Distress during cancer care. NCCN Guidelines for Patients. 2023. Accessed December 15, 2023. https://www.nccn.org/patients/guidelines/content/PDF/distress-patient.pdf
National Comprehensive Cancer Network. Distress management. Version 1.2024. NCCN Guidelines. Updated October 2023. Accessed December 15, 2023. https://www.nccn.org/professionals/physician_gls/pdf/distress.pdf
Office of Disease Prevention and Health Promotion (OASH). Social cohesion. Healthy People 2030. 2021. Accessed December 15, 2023. https://health.gov/healthypeople/priority-areas/social-determinants-health/literature-summaries/social-cohesion
Our epidemic of loneliness and isolation: The U.S. Surgeon General’s advisory on the healing effects of social connection and community. US Department of Health and Human Services. May 2023. Accessed December 15, 2023. https://www.hhs.gov/sites/default/files/surgeon-general-social-connection-advisory.pdf
Roy-Byrne PP. Management of psychiatric disorders in patients with cancer. UpToDate. UpToDate Inc; 2023. Updated September 2023. Accessed December 15, 2023. https://www.uptodate.com/contents/management-of-psychiatric-disorders-in-patients-with-cancer
Saad AM, Gad MM, Al-Husseini MJ, AlKhayat MA, Rachid A, Alfaar AS and Hamoda H. Suicidal death within a year of a cancer diagnosis: A population-based study. Cancer. 2019. 125: 972-979. https://doi.org/10.1002/cncr.31876
Syrjala KL & Chiyon Yi J. Overview of psychosocial issues in the adult cancer survivor. UpToDate. UpToDate Inc; 2023. Updated October 2023. Accessed December 15, 2023. https://www.uptodate.com/contents/overview-of-psychosocial-issues-in-the-adult-cancer-survivor
Last Revised: July 25, 2024
American Cancer Society medical information is copyrighted material. For reprint requests, please see our Content Usage Policy.
American Cancer Society Emails
Sign up to stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society.


