Treatments for Obesity (Weight Loss Treatments)
Excess body weight is linked with an increased risk of many types of cancer. It’s not yet clear if losing weight (on purpose) can lower a person’s cancer risk, but there’s reason to think it might. The American Cancer Society recommends that people try to get to and stay at a healthy weight throughout their lives.
Along with possibly reducing cancer risk, losing weight can have many other health benefits, such as lowering your risk of heart disease and diabetes. Losing even a small amount of weight has health benefits and is a good place to start. People with excess body weight who are trying (or want to try) to lose weight need to know the options available to them.
Why is it so hard to lose weight and keep it off?
Obesity is a chronic (deep-rooted) condition that increases a person’s the risk of having health problems. Losing weight is hard for most people. It can also be hard to maintain weight loss.
Your body’s natural weight range (Set point theory)
One reason weight loss is hard is that your body has built-in ways to resist it. Set point theory suggests that a person’s body has a natural weight range it tries to maintain. This range is established early in life and stays fairly stable over time. However, changes in health can change the body’s set point throughout a person’s life.
This means that when you try to lose weight, your body may respond by slowing your metabolism or increasing hunger to return to its set point. This can make it hard to lose weight and keep it off, even with diet and exercise. But gradual and consistent changes in habits can sometimes help the body adjust to a new, lower set point over time.
Hunger hormones
One of the ways our bodies defend against losing weight is by adjusting levels of certain hormones that can affect appetite. These include:
Ghrelin: A hormone that helps signal that you’re hungry. It’s made in the stomach and intestines (gut) and sends signals through your bloodstream to your brain when it’s time to eat, increasing your appetite. Its levels are highest before a regular meal or if a person hasn’t eaten in a while.
Leptin: A hormone that helps signal when you’re full. It’s made in fat cells (adipose tissue). After a meal, fat cells release leptin into your bloodstream, which signals your brain to stop eating.
Insulin: A hormone made in the pancreas that regulates blood sugar levels and reduces ghrelin levels after you eat. It helps turn food into energy and helps the body’s cells work correctly. When you eat, blood glucose levels increase, which triggers the pancreas to release insulin. Insulin helps blood glucose enter the body’s cells for energy.
Glucagon-like peptide-1 (GLP-1): A hormone made mainly in the intestines that raises insulin levels and slows stomach emptying, which lowers appetite.
Gastric inhibitory polypeptide (GIP): A hormone made in the intestines that is similar to GLP-1. It raises insulin levels and may also affect stomach emptying.
These and other hormones work together to regulate hunger, appetite, and body weight. But changes in health or lifestyle can disrupt this balance, leading to weight gain and making weight loss more challenging.
Methods of weight loss
Losing weight can look different for each person. Different methods of losing weight can include:
- Limiting calories and being physically active, either on one’s own or with professional help
- Intensive behavioral therapy (IBT)
- Weight loss drugs
- Weight loss surgery (bariatric surgery)
Several of these are described below.
Intensive behavioral therapy (IBT)
People often try to eat less or move more with hopes of reaching their goal weight. Some people do achieve their weight goals in this way, either on their own or with the help of a nutritionist or dietitian.
However, a more structured approach to behavior change has shown to be helpful.
Working with a mental health professional (such as a psychologist or weight loss counselor or therapist) can help guide you during a weight loss journey. Intensive behavioral therapy (IBT) combines different types of therapy that focus on changing your thoughts and responses. By adjusting how you think about food and activity, IBT can help you make changes that last.
IBT for weight loss often includes:
- Goal setting
- Dietary changes with food tracking
- Regular physical activity
- Stress management
- Cognitive behavioral therapy (CBT), such as guided relaxation techniques and coping strategies.
IBT programs are offered in many larger hospitals and care centers. The programs often last 1 to 2 years and usually include 12 or more sessions in the first year. They may start with more frequent sessions, and then the sessions may be scheduled less often. Sessions can be done in-person or virtually (online or by telephone).
How effective is IBT?
Research shows that IBT can been helpful for managing problems like depression, anxiety, eating disorders, and alcohol and drug use disorder.
For losing and maintaining weight, IBT can help you change your lifestyle through making better food choices and getting regular physical activity. These lifestyle changes can help you get to and stay at a healthy weight.
Results of studies using IBT for weight loss show that people can lose 5% to 10% of their body weight, which can be helpful in reducing some health risks, like lowering blood pressure and improving hemoglobin A1C levels in people with type 2 diabetes.
Like any program or treatment for weight loss, it may be hard to maintain weight loss once you stop the program.
What are the benefits and risks of using IBT?
An IBT plan includes your goals and helps you reach them. There are multiple parts of IBT that help you adjust to expected lifestyle changes, including:
- Monitoring your own progress, or self-monitoring
- Exercises that are best for you to increase physical activity and strength
- Helping to improve the way you think about food, your body shape and size, and ability to meet your goals
According to the US Preventive Services Task Force, there is no evidence that using IBT for weight loss is risky or harmful. However, finding and accessing IBT programs might be hard for some people. There may be limited or no programs available where you live, or a lack of insurance coverage for the programs.
Weight loss drugs
Medicines to help with weight loss have been prescribed for many years. Weight loss drugs work in different ways. They can:
- Decrease appetite so you don’t feel as hungry
- Control blood glucose (sugar) by helping the pancreas make and release insulin
- Slow the emptying time of the stomach to make you feel full longer
- Work in the brain to decrease food cravings and unpleasant thoughts about eating (commonly called “food noise”)
GLP-1 drugs: semaglutide, tirzepatide, and liraglutide
In recent years, newer drugs called glucagon-like peptide-1 receptor agonists (GLP-1 RAs, GLP-1 drugs, or just GLP-1s) have become available. These drugs generally are more effective and work for more people than older weight loss medicines. They have also been found to improve some chronic health conditions, like diabetes and heart disease.
These drugs work by acting like GLP-1 in the body. They activate the GLP-1 receptor on certain cells, which increases insulin levels and slows gastric (stomach) emptying. This helps lower appetite and makes you feel full for longer.
GLP-1 drugs (such as Ozempic) were originally FDA-approved to treat type 2 diabetes, but some of them are now approved for weight loss (when used along with a low-calorie diet and increased physical activity).
Liraglutide (Saxenda)
- How it works: Activates GLP-1 receptors in the body
- Year FDA approved (for weight loss): 2014
- How taken: Once a day injection
- Average weight loss: 8% of body weight
- Common side effects: Nausea, vomiting, diarrhea, constipation, increased heart rate, dizziness, mood changes, fatigue, low blood glucose
Semaglutide (Wegovy)
- How it works: Activates GLP-1 receptors in the body
- Year FDA approved (for weight loss): 2021
- How taken: Once a week injection
- Average weight loss: 15% of body weight
- Common side effects: Nausea, vomiting, diarrhea, constipation, abdominal (belly) pain, headache, heartburn or reflux, dizziness, mood changes, fatigue, low blood glucose
Tirzepatide (Zepbound)
- How it works: Activates GLP-1 and GIP receptors in the body
- Year FDA approved (for weight loss): 2022
- How taken: Once a week injection
- Average weight loss: 20% of body weight
- Common side effects: Nausea, vomiting, diarrhea, constipation, abdominal (belly) pain, heartburn or reflux, dizziness, mood changes, fatigue, low blood glucose, redness at injection site, allergic reactions
How effective are GLP-1 drugs, and how long are they taken?
Weight loss results can vary based on the type and dosage of GLP-1 drug used. For the treatment of obesity, many experts recommend that these drugs be used in addition to behavioral changes that include eating a healthy diet and getting plenty of physical activity. This may also help decrease side effects that might happen when starting one of these drugs. Therapy (such as intensive behavioral therapy) can also help add to the success of treatment.
The amount of weight loss with GLP-1 drugs varies for people. Most weight loss occurs within the first year of starting one of these drugs. Weight loss slows down after the first year, and it can be harder to lose more weight.
Studies on long-term effects of GLP-1 drugs have found that some people regain weight after they stop taking these medicines. Because of this, doctors might recommend staying on these drugs (perhaps at a lower dose) long term to maintain weight loss.
Can GLP-1 drugs affect cancer risk?
So far, the answer to this question isn’t clear. Researchers continue to study how anti-obesity medicines might affect cancer risk. Results have been mixed so far, based on the cancer type studied.
- Some studies have suggested that the use of GLP-1 drugs might lower the risk for breast, prostate, lung, pancreatic, colon and liver cancers, as well as basal cell carcinoma of the skin.
- In some animal studies of GLP-1 drugs, a higher risk of a rare type of thyroid cancer (medullary thyroid cancer, or MTC) has been found. Because of this, these drugs should not be used by people with a personal or family history of MTC or a rare genetic disorder called multiple endocrine neoplasia syndrome type 2 (MEN2).
Talk to your health care team about the best options for you to manage your weight and have long lasting results.
Other weight loss drugs
In addition to the newer GLP-1 drugs, there are other FDA-approved drugs that can help treat obesity in some people.
Orlistat (Alli, Xenical)
- How it works: Slows or blocks the absorption of fat from foods during digestion
- Year FDA approved: 1999
- How taken: As a capsule by mouth
- Average weight loss: 2.8% to 4.8% of body weight
- Common side effects: Abdominal (belly) cramps, gas, oily spotting of stool, and bowel incontinence (lack of self-control of stool)
Phentermine/topiramate (Qsymia)
- How it works: Combines 2 medicines that affect chemicals in the brain to lower appetite and make you feel more full
- Year FDA approved: 2012
- How taken: As a capsule by mouth
- Average weight loss: 5% to 10% of body weight
- Common side effects: Dry mouth, changes in taste, constipation, mood changes, depression, anxiety, sleep problems, increased heart rate
Bupropion/naltrexone (Contrave)
- How it works: Combines 2 medicines that help lower appetite and food cravings
- Year FDA approved: 2014
- How taken: As a pill by mouth
- Average weight loss: 6% of body weight
- Common side effects: Nausea, constipation, headache, vomiting, dizziness, sleep problems, and dry mouth. Blood pressure and heart rate may increase during the first 12 weeks of treatment.
Bariatric surgery (weight loss surgery)
Bariatric surgery can help people with obesity lose weight and improve their health and quality of life. These surgeries are done on the stomach or intestines to induce weight loss. Bariatric surgery that leads to weight loss can help manage or even reverse some health conditions, such as diabetes and high blood pressure.
How effective is bariatric surgery?
For some types of bariatric surgery, people may lose about 25% body fat and are likely to keep it off for at least 5 years. It’s important to know that the full results of surgery might take some time. Initial weight loss may be rapid for a few months after surgery, but it can slow or stop after a period of time. A person may not see their desired weight loss until a year or longer after surgery. However, research shows people have an overall sense of improved well-being and quality of life after having bariatric surgery.
When is bariatric surgery recommended?
Bariatric surgery may be recommended when diet and exercise changes are not effective.
The American Society for Metabolic and Bariatric Surgery (ASMBS) is the largest professional group of bariatric surgeons in the US. The ASMBS has recommendations for bariatric surgery for people who have a higher BMI level but the recommendations can vary for people who have obesity-related conditions. In general, the ASMBS recommends bariatric surgery only for people with a BMI of 35 or more, or for people with a BMI of 30 or more who also have certain obesity-related conditions, such as diabetes. It’s best to talk with your doctor for more information about when weight loss surgery may be recommended.
The ASMBS has endorsed several types of surgeries for weight loss. If you’re thinking about getting weight loss surgery, the first step is to talk to your doctor about the benefits and risks, and which procedure might be best for you.
Planning for bariatric surgery usually takes several months after the initial consult with a bariatric team. This team consists of doctors, nurses, case managers, pharmacists, dietitians, social workers, and psychologists, who work directly with the person throughout their weight loss journey.
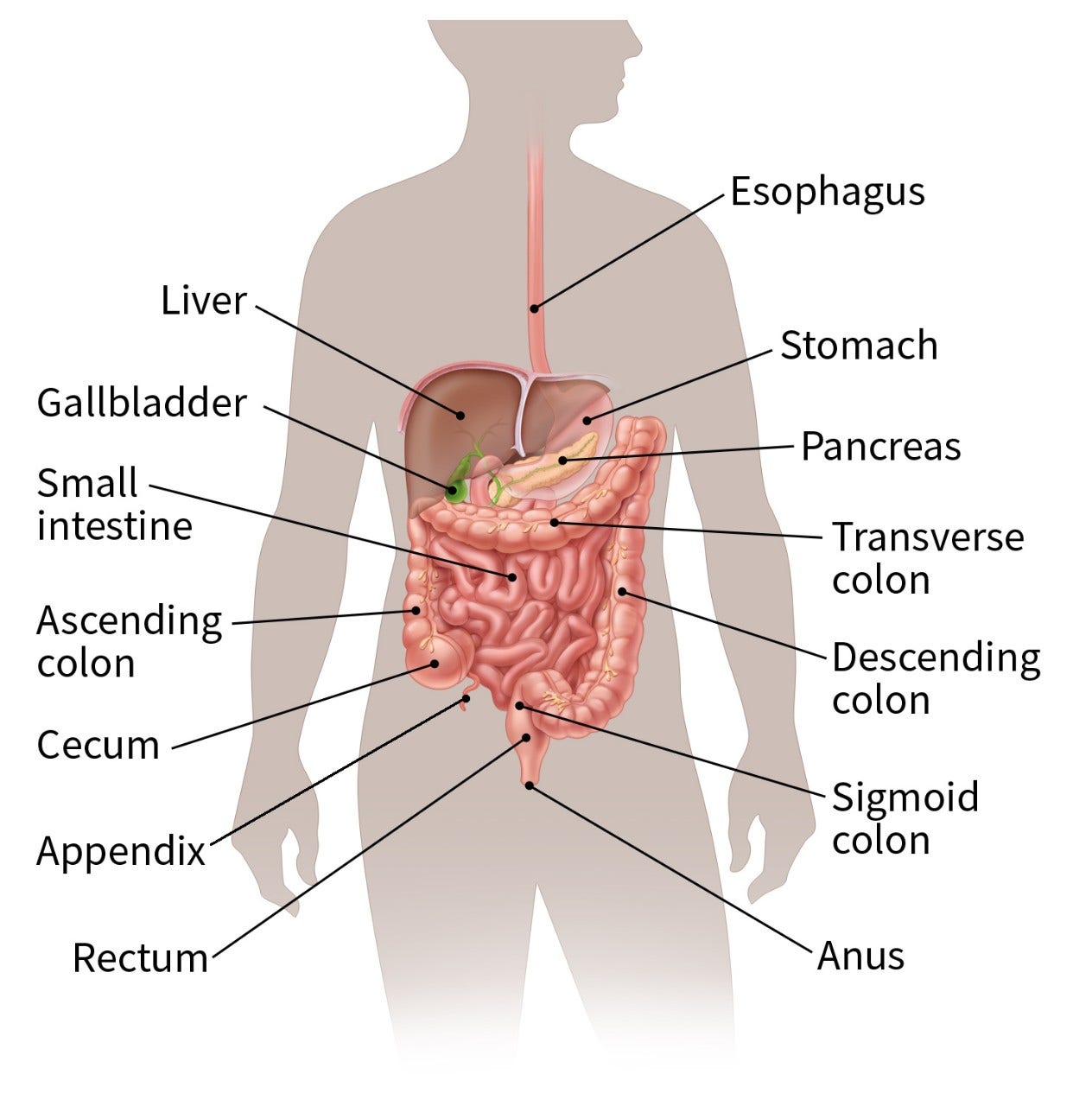
As you learn about the procedures, it may help to look at anatomy images along with a 3-D tour of the digestive system to help you see and understand the different parts of the digestive system, also called the gastrointestinal (GI) system.
Gastric sleeve (sleeve gastrectomy)
This is the most common type of bariatric surgery in the US. The procedure removes most of the stomach and leaves a small, banana-size shape to the stomach. The “new” stomach is much smaller and holds much less food and fluids. This limits how much the person can eat in one sitting after the surgery. It also helps decrease feelings of being hungry because the stomach size is smaller.
- Effect: Expected weight loss of about 25% of body weight at 12 months after surgery
- Benefits:
- Procedure takes a short time and is simpler than others.
- Weight loss is usually sustained at 5 years.
- Risks:
- The procedure cannot be reversed.
- It may trigger new problems like heartburn or gastric reflux or can also make these problems worse if you already have them.
Roux-en-Y gastric bypass (gastric bypass)
This procedure involves dividing the stomach into two parts – the upper part becomes a small pouch, and the lower part becomes a larger pouch. The small intestine is also divided, creating a new branch that it is connected to the smaller upper stomach pouch. The start of the resulting small intestine is in the shape of a Y, with connections to each pouch.
After the procedure, when food is swallowed it goes into the small pouch, then directly into the new branch of the small intestine. Food will bypass the large lower stomach pouch, as well as the first part of the small intestine that’s still connected to it. This limits how much the person can eat in one sitting after the surgery, as well as how much is absorbed by the small intestine. It also helps decrease feelings of being hungry.
- Effect: Expected weight loss of about 25% of body weight at 12 months after surgery
- Benefits:
- Weight loss is usually sustained at 5 years.
- Procedure is reversible.
- Risks:
- This is a more complex operation than the others.
- Is more likely than the other procedures to cause problems due to the body not being able to absorb some of the recommended vitamins and minerals it needs.
- It increases the risk for small bowel obstruction and stomach ulcers.
- It may cause dumping syndrome – when food moves too fast through the digestion process, causing nausea, bloating, cramps, and diarrhea after eating and drinking.
Adjustable gastric band (lap-band surgery)
In this procedure, a silicone band is placed around the upper part of your stomach, creating a small pouch above the band. The band can be adjusted (using a syringe to add or remove fluid from the band) or removed. It may need a few adjustments during the first year. This procedure is less common than gastric sleeve or gastric bypass procedures.
- Effect: Expected weight loss is less than gastric sleeve or Roux-en-Y gastric bypass.
- Benefits:
- The band can be adjusted and is removable.
- There’s less chance of problems right after surgery.
- There’s less risk for a lack of vitamins and minerals being absorbed.
- Risks:
- The band may move and need to be adjusted.
- Sometimes the band can damage the wall of the stomach.
- Some people might have swallowing problems and enlargement of the esophagus or the upper stomach pouch.
- There is a higher chance of people not tolerating the band compared to other surgeries.
Other weight loss surgeries
Biliopancreatic diversion with duodenal switch (BPD-DS) and single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S) are newer procedures that are not performed as often in the US. They are typically more complex and can have a higher risk of serious complications.
Can bariatric surgery affect cancer risk?
Bariatric surgery and cancer risk continue to be studied by researchers. Studies on bariatric surgery and cancer risk have had mixed findings.
- Some studies have suggested that bariatric surgery can help lower a person’s risk of breast, endometrial (uterus), colorectal, liver, pancreatic, gallbladder, and ovarian cancers, as well as multiple myeloma. Bariatric surgery has not been found to lower the risk of gastric (stomach), esophageal, prostate, thyroid, or kidney cancer. A few studies have suggested that it might increase the risk of some cancers.
- In people who have cancer, bariatric surgery has been linked with a lower risk of developing a second cancer and dying from cancer.
- Written by
- References

The American Cancer Society medical and editorial content team
Our team is made up of doctors and oncology certified nurses with deep knowledge of cancer care as well as editors and translators with extensive experience in medical writing.
Angrisani L, Santonicola A, Iovino P, et al. IFSO Worldwide Survey 2016: primary, endoluminal, and revisional procedures. Obesity Surgery. 2018;28(12):3783–3794. doi: 10.1007/s11695-018-3450-2.
Bezin J, Gouverneur A, Penichon M, et al. GLP-1 receptor agonists and the risk of thyroid cancer. Diabetes Care. 2023; 46(2):384-390.
Brandfon S, Eylon A, Khanna D, Parmar MS. Advances in anti-obesity pharmacotherapy: Current treatments, emerging therapies, and challenges. Cureus. 2023;15(10):e46623. Published 2023 Oct 7. doi:10.7759/cureus.46623.
Caruso A, Gelsomino L, Panza S, et al. Leptin: A heavyweight player in obesity-related cancers. Biomolecules. 2023;13(7):1084.
Eisenberg D, Shikora SA, Aarts E, et al. 2022 American Society for Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO): Indications for Metabolic and Bariatric Surgery. Surg Obes Relat Dis. 2022 Dec;18(12):1345-1356.
Elmaleh-Sachs A, Schwartz JL, Bramante CT, et al. Obesity management in adults: A review. JAMA. 2023 Nov 28;330(20):2000-15. doi:10.1001/jama.2023.1989.
Ganipisetti VM, Bollimunta P. Obesity and set-point theory. [Updated 2023 Apr 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan. Accessed at https://www.ncbi.nlm.nih.gov/books/NBK592402/ on November 25, 2024.
Hinte LC, Castellano-Castillo D, Ghosh A, et al. Adipose tissue retains an epigenetic memory of obesity after weight loss. Nature (2024). https://doi.org/10.1038/s41586-024-08165-7
Ibrahim SS, Ibrahim RS, Arabi B, et al. The effect of GLP-1R agonists on the medical triad of obesity, diabetes, and cancer. Cancer Metastasis Rev. Published online May 27, 2024. doi:10.1007/s10555-024-10192-9.
Jacob JJ, Isaac R. Behavioral therapy for management of obesity. Indian Journal of Endocrinology and Metabolism. 2012 Jan 1;16(1):28-32. DOI: 10.4103/2230-8210.91180.
Khalilov R, Abdullayeva S. Mechanisms of insulin action and insulin resistance. Advances in Biology & Earth Sciences. 2023;8(2).
Lim RB. Bariatric procedures for the management of severe obesity: Descriptions. UpToDate. 2023.
Lin C, et al. Comparative risk of obesity-related cancer with glucagon-like protein-1 receptor agonists vs. bariatric surgery in patients with BMI >35. Journal of Clinical Oncology. 2024; 42(16):suppl. doi.org/10.1200/JCO.2024.42.16_suppl.10508.
López M, Nogueiras R. Ghrelin. Current Biology. 2023;33(21):R1133-1135. DOI: 10.1016/j.cub.2023.09.009
Perreault L, Reid TJ. Obesity in adults: Drug therapy. UpToDate. 2024.
Sun Y, Liu Y, Dian Y, Zeng F, Deng G, Lei S. Association of glucagon-like peptide-1 receptor agonists with risk of cancers-evidence from a drug target Mendelian randomization and clinical trials. Int J Surg. 2024;110(8):4688-4694. Published 2024 Aug 1. doi:10.1097/JS9.0000000000001514.
US Preventive Services Task Force. About prevention taskforce. U.S. Protective Services Task Force. Accessed October 4, 2024. https://www.uspreventiveservicestaskforce.org/apps/about.jsp.
Wilson RB, Lathigara D, Kaushal D. Systematic review and meta-analysis of the impact of bariatric surgery on future cancer risk. Int J Mol Sci. 2023; 24(7):6192. https://doi.org/10.3390/ijms24076192.
Last Revised: December 20, 2024
American Cancer Society medical information is copyrighted material. For reprint requests, please see our Content Usage Policy.
More Resources
More Interactive Tools
American Cancer Society Emails
Sign up to stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society.






