Health Risks of Smoking Tobacco
Tobacco use remains the leading preventable cause of disease and death in the United States. About 480,000 people die from cigarette smoking each year in the US. Many of those people die from cancer.
But smoking does more than just cause cancer. It can also cause a number of other diseases and can damage nearly every organ in your body including your lungs, heart, blood vessels, reproductive organs, mouth, skin, eyes, and bones.
On average, people who smoke die about 10 years earlier than people who have never smoked.
Learn more about the health risks of smoking tobacco.
- How smoking tobacco affects your cancer risk
- How smoking tobacco damages your lungs
- How smoking tobacco affects your heart and blood vessels
- Smokeless tobacco and heart disease
- How using tobacco can affect your sex life and reproductive system
- Other ways tobacco use affects your health
- How using tobacco can affect children and teens
- Learn more
How smoking tobacco affects your cancer risk
Smoking causes about 20% of all cancers and about 30% of all cancer deaths in the United States.
About 80% of lung cancers (and about 80% of all lung cancer deaths) are due to smoking. Lung cancer is the leading cause of cancer death in people in the United States.
Smoking also increases the risk for cancers of the:
- Mouth
- Larynx (voice box)
- Pharynx (throat)
- Esophagus
- Kidney
- Cervix
- Liver
- Bladder
- Pancreas
- Stomach
- Colon/rectum
- And acute myeloid leukemia
Learn more about these cancers in: Cancer Types
Studies indicate that smoking may also increase the risk for fatal prostate cancer and a rare type of ovarian cancer.
Cigarettes, cigars, and pipes can all cause cancer. There is no safe form of tobacco smoke.
How smoking tobacco damages your lungs
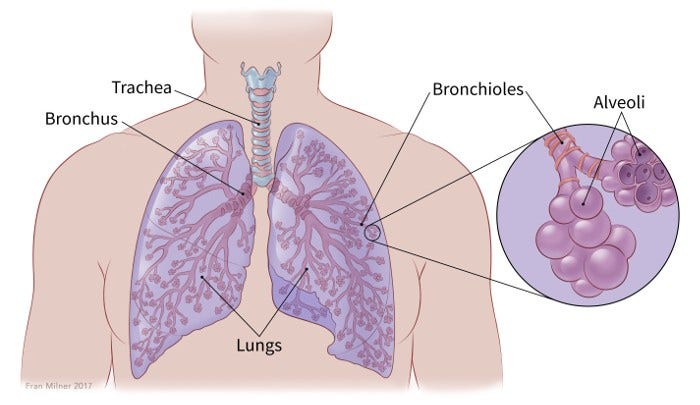
Smoking damages the airways and small air sacs in your lungs. This damage starts soon after you start smoking and gets worse as long as you continue to smoke. But it may take years for symptoms of this damage to be severe enough for lung disease to be diagnosed.
Smoke damage in your lungs can lead to serious long-term lung diseases like chronic obstructive pulmonary disease (COPD). Smoking can also increase the risk of lung infections like pneumonia and tuberculosis. It can worsen some existing lung diseases, such as asthma.
COPD
Smoking is by far the most common cause of COPD. The risk goes up the more you smoke and the longer you smoke.
COPD is one of the leading causes of death in the United States. It includes both chronic bronchitis and emphysema. Most people with COPD have both of these conditions, but how severe they are varies from person to person.
When you have COPD, the small airways in your lungs are damaged. This damage makes it hard for your lungs to get oxygen to the rest of your body. Early symptoms can include noises in your chest (such as wheezing, rattling, or whistling), shortness of breath when you are active, and coughing up mucus (phlegm).
Over time, COPD can also make it hard to breathe when you are at rest, sometimes even if you are getting oxygen. COPD tends to get worse over time, especially if you continue to smoke. There is no cure for COPD, but some medicines might help with symptoms.
Chronic bronchitis
Chronic bronchitis is common in people who smoke for a long time. When you have chronic bronchitis, your airways make too much mucus, so you feel like you have to cough it out. Your airways become inflamed (swollen), and the cough becomes chronic (long-lasting).
The symptoms can get better at times, but the cough keeps coming back. Over time, the airways can get blocked by scar tissue and mucus, which can lead to bad lung infections (pneumonia).
There’s no cure for chronic bronchitis. But quitting smoking can help the damage from getting worse and keep symptoms under control.
Emphysema
In emphysema, the walls between the tiny air sacs in the lungs break down, which creates larger but fewer air sacs. This lowers the amount of oxygen reaching the blood. Over time, these sacs can break down so that a person with emphysema might struggle to get enough air, even when at rest.
People with emphysema are at risk for many other problems, including pneumonia. In later stages of the disease, a person often needs supplemental oxygen to help them breathe.
Emphysema can’t be cured, but it can be treated and slowed down if the person stops smoking.
Why do people who smoke have “smoker’s cough?”
Tobacco smoke has many chemicals and particles that can irritate the upper airways and the lungs. When you inhale these substances, your body tries to get rid of them by making mucus and causing a cough.
People who smoke will often have a long-lasting cough. This is sometimes called a “smoker’s cough,” and it is often worse in the morning. This chronic cough happens for many reasons.
Normally, tiny hair-like structures in the airways (called cilia) help sweep harmful material out of the lungs. But tobacco smoke slows this sweeping action, so some of the mucus and particles in the smoke stay in the lungs and airways. While a person sleeps (and doesn’t smoke), some cilia recover and start working again. After waking up, the person coughs because their lungs are trying to clear away the irritants and mucus that built up from the day before.
“Smoker’s cough” can be an early sign of COPD.
How smoking tobacco affects your heart and blood vessels
Smoking tobacco damages your heart and blood vessels (cardiovascular system). This increases your risk of heart disease and stroke.
Coronary heart disease (CHD)
Coronary heart disease is when the arteries of your heart become narrow and can’t provide your heart muscle with enough oxygen. CHD is the main cause of heart attacks, and it’s the leading cause of death in the United States. Smoking increases your risk of CHD by damaging the blood vessels that supply the heart. .
Heart attacks and strokes
Heart attacks and strokes are more common in people who smoke. Smoking causes high blood pressure, lowers your ability to exercise, and makes your blood more likely to clot. It also lowers the levels of HDL cholesterol (good cholesterol) in your blood. All of this increases the risk of heart attacks and strokes.
Peripheral arterial disease (PAD)
Peripheral arterial disease is also more common in people who smoke. In PAD, plaque builds up in the arteries that carry blood to your head, organs, and limbs. This increases your risk of heart disease, heart attack, and stroke. It can also cause pain or weakness in your arms and legs, making it harder to walk and do usual activities.
Aortic aneurysm
Aortic aneurysm has been linked with tobacco smoking. This is a balloon-like bulge in the aorta, the main artery carrying blood from your heart to your other organs. It is caused by a weakening of the aorta wall. Aortic aneurysms can grow larger over time. They can be life-threatening if they rupture (break open).
Peripheral vascular disease (PVD)
Peripheral vascular disease is when blood flow to your arms and legs is decreased. This can lead to pain in your legs when you walk. It may also lead to open sores that don’t heal.
Because smoking affects blood flow, it can lower your body’s ability to heal from cuts. This is why many doctors won’t do certain operations on patients unless they stop smoking.
Smokeless tobacco and heart disease
Most research has focused on the impact of smoking tobacco on heart health. But smokeless tobacco can also increase your risk of heart disease.
Smokeless tobacco has been linked to a higher risk of death from coronary heart disease and stroke. This appears to be related not just to nicotine, but also to other chemicals found in smokeless tobacco products.
Learn more: Health Risks of Smokeless Tobacco
How using tobacco can affect your sex life and reproductive system
Using tobacco can affect the reproductive health and sexual function of both men and women. It can also affect fertility, pregnancy, labor, and birth.
Women
Women who smoke are more likely to have trouble getting pregnant.
If you use tobacco while you’re pregnant, your fetus is exposed to nicotine and other chemicals that are known to cause genetic defects.
Using tobacco while pregnant puts you at higher risk of:
Ectopic pregnancy
This happens when an embryo implants outside your uterus. It can be life-threatening for the pregnant woman.
Problems with the placenta
The placenta is an organ that connects your body to your fetus during pregnancy. Using tobacco when you are pregnant might cause the placenta to be too far down in your uterus (placenta previa). Or, it might separate from your uterus too early (placental abruption).
These can lead to serious bleeding, early delivery (premature birth), or other problems with the delivery. In some cases, you might need an emergency Caesarean section (C-section).
Prelabor rupture of membranes (PROM)
The membranes (a fluid-filled sac that holds the fetus) may break before the fetus is full term. This is called prelabor rupture of membranes (PROM). It can lead to an early or difficult labor, infection, and death of the fetus.
Premature birth, miscarriage, and birth defects
If you smoke while pregnant, you are more likely to have complications that affect your baby. This might include:
- Low birth-weight baby
- Premature birth
- Miscarriage or stillbirth
- Birth defects, including: cleft lip, cleft palate, internal organ deformities, or limb deformities
Babies of mothers who smoke during and after pregnancy are also more likely to die from sudden infant death syndrome (SIDS). These babies are also more likely to get lung infections, asthma, and have problems in school.
Men
Smoking can damage blood vessels anywhere in your body. Increased blood flow to the penis is a key part of male erections. Men who smoke have a higher risk of erectile dysfunction because blood vessels become narrower. The risk of erectile dysfunction increases the more you smoke and the longer you smoke.
Smoking can also make your sperm less healthy. This can reduce fertility (make it harder for you to father a child).It can also increase the risk of your partner having miscarriages and your child having birth defects.
Other ways tobacco use affects your health
Smoking and using other tobacco products harms nearly every organ in your body. It can affect your health in many ways.
Here are a few examples of the other ways using tobacco can affect your health:
- Increased risk of gum disease and tooth loss
- Lowered immune system function
- Increased risk of type 2 diabetes
- Decreased sense of smell and taste
- Premature aging of your skin
- Bad breath and stained teeth
- Lower bone density (thinner bones), which means a higher risk for broken bones, including hip fracture
- Higher risk of rheumatoid arthritis
- Increased risk for cataracts (clouding of the lenses of your eyes)
- Increased risk for age-related macular degeneration, which can lead to blindness
- Slower healing of wounds
Many of the health problems linked to smoking can also lower your quality of life. Tobacco-related illness can make it harder to breathe, get around, work, or play. Quitting tobacco, especially at a younger age, can reduce tobacco-related disability.
Learn more: How to Quit Using Tobacco
How using tobacco can affect children and teens
Smoking cigarettes and using other tobacco products can cause health problems in children and teens. The same is true of children who are exposed to secondhand smoke from people in their home, in the car, or other places where smoking is allowed.
Over time, children and teens who smoke cigarettes, use other tobacco products, or are exposed to secondhand smoke can develop serious health problems, including later in life as adults.
Nicotine addiction
One of the most serious problems for children and teens who use tobacco is nicotine addiction. This often leads to long-term tobacco use as kids get older.
Brain development
Nicotine can also harm the brain development of children and teens. It’s important to know that most e-cigarettes and similar products also have nicotine.
Physical health problems
Children and teens who use tobacco, or who are regularly exposed to secondhand smoke, tend to have more health problems than kids who don’t.
These health problems can include:
- Coughing spells
- Shortness of breath, even when not exercising
- Wheezing or gasping
- Increased phlegm (mucus)
- Respiratory illnesses that are worse and happen more often
- Worse cold and flu symptoms
- More frequent headaches
- Reduced physical fitness
- Poor lung growth and function, which increases the risk of COPD later in life
Tobacco use and harmful behaviors in teens
Research has shown that teen tobacco users are more likely to use alcohol, cannabis, and illegal drugs compared to teens who don’t use tobacco.
Teens who smoke are more likely to have mental health problems such as depression, anxiety, ADHD, and other disorders that can cause the teen to be disruptive. This doesn’t necessarily mean that tobacco use causes these mental health problems or behaviors. But the behaviors are more commonly seen in teens who use tobacco.
In addition, using e-cigarettes (also known as vaping) might play a part in a child or teenager wanting to experiment with other tobacco products.
Learn more
- Written by
- References

Developed by the American Cancer Society medical and editorial content team with medical review and contribution by the American Society of Clinical Oncology (ASCO).
Al-Bashaireh AM, Haddad LG, Weaver M, Chengguo X, Kelly DL, Yoon S. The Effect of Tobacco Smoking on Bone Mass: An Overview of Pathophysiologic Mechanisms. J Osteoporos. 2018;2018:1206235. Published 2018 Dec 2. doi:10.1155/2018/1206235
American Cancer Society. Cancer Prevention & Early Detection Facts & Figures 2023-2024. Accessed at https://www.cancer.org/research/cancer-facts-statistics/cancer-prevention-early-detection.html on September 27, 2024.
American Cancer Society. Cancer Facts & Figures 2024. Accessed at https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/2024-cancer-facts-figures.html on September 27, 2024.
Aune D, Schlesinger S, Norat T, Riboli E. Tobacco smoking and the risk of abdominal aortic aneurysm: a systematic review and meta-analysis of prospective studies. Sci Rep. 2018;8(1):14786. Published 2018 Oct 3. doi:10.1038/s41598-018-32100-2
Centers for Disease Control and Prevention (CDC). Burden of Cigarette Use in the US. Accessed at https://www.cdc.gov/tobacco/campaign/tips/resources/data/cigarette-smoking-in-united-states.html on September 25, 2024.
Centers for Disease Control and Prevention (CDC). Cigarette Smoking. Accessed at https://www.cdc.gov/tobacco/about/index.html on September 27, 2024.
Centers for Disease Control and Prevention (CDC), National Center for Chronic Disease Prevention and Health Promotion, and Office on Smoking and Health. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. 2010. Atlanta (GA): Centers for Disease Control and Prevention. Accessed at https://www.ncbi.nlm.nih.gov/books/NBK53017 on September 27, 2024.
Centers for Disease Control and Prevention (CDC). Tips From Former Smokers: Pregnancy. Accessed at https://www.cdc.gov/tobacco/campaign/tips/diseases/pregnancy.html on October 1, 2024.
Drope J, Cahn Z, Kennedy R, et al. Key issues surrounding the health impacts of electronic nicotine delivery systems (ENDS) and other sources of nicotine. CA Cancer J Clin. 2017;87(6):449-471. Accessed at https://doi.org/10.3322/caac.21413 on October 12, 2020.
Gould GS, Havard A, Lim LL, The Psanz Smoking In Pregnancy Expert Group, Kumar R. Exposure to Tobacco, Environmental Tobacco Smoke and Nicotine in Pregnancy: A Pragmatic Overview of Reviews of Maternal and Child Outcomes, Effectiveness of Interventions and Barriers and Facilitators to Quitting. Int J Environ Res Public Health. 2020;17(6):2034. doi:10.3390/ijerph17062034
Gupta R, Gupta S, Sharma S, Sinha DN, Mehrotra R. Risk of Coronary Heart Disease Among Smokeless Tobacco Users: Results of Systematic Review and Meta-Analysis of Global Data. Nicotine Tob Res. 2019;21(1):25-31. doi:10.1093/ntr/nty002
Hornstein MD, Gibbons WE, Schenken RS. Natural fertility and impact of lifestyle factors. In, UpToDate, Post TW (Ed). Accessed at uptodate.com on October 1, 2024.
Islami F, Marlow EC, Thomson B, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States, 2019. CA Cancer J Clin. 2024;74(5):405-432. doi:10.3322/caac.21858
Lai S, Lai H, Page JB, McCoy CB. The association between cigarette smoking and drug abuse in the United States. J Addict Dis. 2000;19(4):11-24. doi:10.1300/J069v19n04_02
McGrath-Morrow SA, Gorzkowski J, Groner JA, et al. The Effects of Nicotine on Development. Pediatrics. 2020;145(3):e20191346. doi:10.1542/peds.2019-1346
National Institutes of Health. National Heart, Lung, and Blood Institute. How Does Smoking Affect the Heart and Blood Vessels? Accessed at https://www.nhlbi.nih.gov/health/heart/smoking on September 27, 2024.
Practice Committee of the American Society for Reproductive Medicine. Electronic address: asrm@asrm.org; Practice Committee of the American Society for Reproductive Medicine. Smoking and infertility: a committee opinion. Fertil Steril. 2018;110(4):611-618. doi:10.1016/j.fertnstert.2018.06.016
Rodriguez D. Cigarette and tobacco products in pregnancy: Impact on pregnancy and the neonate. In, UpToDate, Post TW (Ed). Accessed at uptodate.com on October 1, 2024.
Rosen RC, Khera M. Epidemiology and etiologies of male sexual dysfunction. In, UpToDate, Post TW (Ed). Accessed at uptodate.com on October 1, 2024.
Rostron BL, Chang JT, Anic GM, et al. Smokeless tobacco use and circulatory disease risk: a systematic review and meta-analysis. Open Heart 2018;5:e000846. doi: 10.1136/openhrt-2018-000846
US Department of Health & Human Services. The Health Consequences of Smoking---50 Years of Progress: A Report of the Surgeon General. 2014. Accessed at https://www.ncbi.nlm.nih.gov/books/NBK179276/pdf/Bookshelf_NBK179276.pdf on September 27, 2024.
Last Revised: November 19, 2024
American Cancer Society medical information is copyrighted material. For reprint requests, please see our Content Usage Policy.
American Cancer Society Emails
Sign up to stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society.


