Not Enough Females Are Being Screened for Cervical Cancer
2025-2026 Cancer Prevention & Early Detection report says cervical cancer prevention needs urgent attention. Good news: Fewer people smoke than ever before.
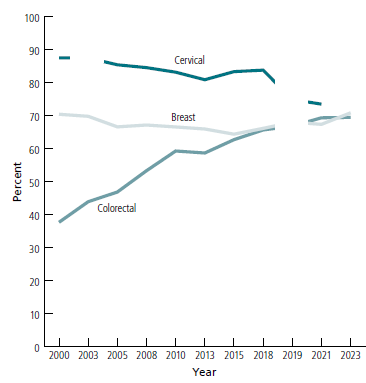
Trends in Screening for Breast, Cervical, and Colorectal Cancer, in the US, 2000-2023*#
This graph shows how the percentage of people being screened for breast, cervical, and colorectal cancer changed from before the COVID-19 pandemic (2019) to after it (2021-2023). Only cervical cancer screening hasn’t rebounded to pre-COVID-19 levels. Source: Cancer Prevention & Early Detection Facts & Figures 2025-2026
Every 2 years, researchers from the American Cancer Society (ACS) publish a comprehensive report using data from multiple national and state surveys about how many adults in the United States report behaviors that can affect their cancer risk or help find it early—because these efforts are essential to reduce the cancer burden.
The latest ACS review of cancer prevention and early detection evaluates the years before (2019), during (2020-2021), and after the COVID-19 pandemic (2023) in the US. Progress was mixed. Smoking prevalence during the pandemic was at an historic low, and fewer teens used e-cigarettes. But more young adults are using e-cigarettes, and obesity rates remained high. In terms of cancer screening and early detection:
- Cervical cancer screening rates were lower during the pandemic than before it, and still haven't rebounded, which unfortunately is a continuation of a declining pattern for the past 20 years.
- Breast and colorectal cancer screening rebounded after declining or stalling during the pandemic.
- HPV vaccination rates were flat during and after the pandemic departing from previously increasing trends.
The current findings are published in the journal Cancer Epidemiology, Biomarkers, & Prevention, a publication of the American Association for Cancer Research (AACR) as well as in the ACS report Cancer Prevention and Early Detection Facts & Figures, 2025-2026. The review is one of the only sources that looks at the major modifiable cancer risk factors in addition to HPV vaccination and cancer screening test use at both the national and state levels.
According to a previous ACS study, about 40% of cancer cases in the US are attributable to potentially modifiable risk factors, which include cigarette smoking, carrying excess body weight, drinking alcohol, physical inactivity, eating unhealthily, excessive ultraviolet radiation exposure, and 7 cancer-causing infections. That means that the implementation of national, state, or private preventive initiatives could substantially reduce the US cancer burden.
HPV vaccination rates for adolescents increased before the pandemic but did not change through 2023.
The human papillomavirus (HPV) vaccine currently used in the US has the potential to prevent about 90% of HPV-caused cancers. All females also need to know that HPV vaccination does not replace cervical cancer screening.
Here are some key statistics.
Before the pandemic: HPV vaccination in adolescents, age 13 to 17, increased significantly between 2019 and 2021.
After the pandemic: Vaccination prevalence has remained unchanged, through 2023.
Cervical cancer screening rates declined during the COVID-19 pandemic and have not returned to their pre-pandemic levels.
Persistent human papillomavirus (HPV) infection causes almost all cervical cancers. Cervical cancer screening is recommended for females ages 21 to 65. Compared to 30 years ago, cervical cancer incidence and death rates are half of what they were—and that’s due to screening.
Cervical cancer could become a thing of the past in the US if all females were current with HPV vaccination recommendations and cervical cancer screening guidelines. Females need them both. Vaccination doesn't replace the need for screening because the vaccine protects against most, but not all, HPV-caused cancers.”

Trends in Cervical Cancer Screening, Ages 21 to 65, by Race/Ethnicity, 2000-2021*
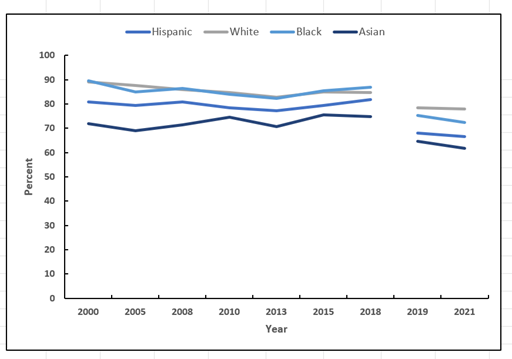
This graph shows the percentage of women who were screened for cervical cancer from the years 2000 to 2021 for Asian, Black, Hispanic, and White females ages 21 to 65. Screening rates are declining for females of all races. Source: Cancer Prevention & Early Detection Facts & Figures 2025-2026
Here are some interesting facts about cervical cancer screening both before and after the pandemic years:
Prevalence for Cervical Cancer Screening Compared with Breast and Colorectal Screenings
See the graph at the top of this article, Trends in Screening for Breast, Cervical, and Colorectal Cancer, in the US, 2000-2023.
Before the pandemic: From the 2000 until the start of the COVID-19 pandemic, a higher percentage of people were up to date with the recommended cervical cancer (dark teal) screening guidelines than were up to date with recommended screenings for breast (light teal/gray) or colorectal cancer (teal).
After the pandemic: The gap in up-to-date screening prevalence between the 3 types of cancer greatly narrowed because cervical cancer screening declined sharply during the COVID-19 pandemic, and, per another ACS study, has yet to rebound after the pandemic.
Prevalence of Cervical Cancer Screening by Race
See the graph above, Trends in Cervical Cancer Screening, Ages 21 to 65, by Race/Ethnicity, 2000-2021.
Before the pandemic: In 2019, more Black (aqua blue) and White (gray) females were up to date with the recommended cervical cancer screening guidelines than Hispanic (dark blue) or Asian females (navy blue/black).
During the pandemic: Black and White females were still more likely to be up to date with cervical cancer screening guidelines than Hispanic and Asian females. The gap between White and Asian females widened due to the decline in screening for Asian females. However, the gaps between Black and Hispanic females narrowed because the screening prevalence for Black females declined.
Breast cancer and colorectal cancer screening prevalence after the pandemic (2023) rebounded and exceeded the levels before (2019) it.
See the graph at the top of this article, Trends in Screening for Breast, Cervical, and Colorectal Cancer, in the US, 2000-2023.
Before the pandemic: The percentage of females getting screened for breast cancer (light teal/gray) gradually declined for years until around 2015, when it almost merged with the percentage of people getting screened for colorectal cancer (teal), which had been increasing for years.
During the pandemic: Breast cancer screening rates dropped, and colorectal cancer screening rates remained flat, departing from prior improvements.
After the pandemic: Both breast cancer and colorectal cancer screening prevalence had rebounded from trends during the pandemic and surpassed pre-pandemic levels.
Tobacco use has declined in the US for decades but still remains the most preventable cause of death in the US.
Cigarette smoking increases the risk for lung cancer, as well as about a dozen other types of cancer. Quitting smoking reduces the risk of developing all cancers caused by smoking.
Here are some of the study’s key statistics from the 2022 to 2023 data for US adults.
Cigarette smoking reached an historic low in 2023. Smoking prevalence peaked at 42% of the US population in 1965. Before the COVID-19 pandemic, it had declined to 14.2%. After it, in 2023, 11% of people in the US smoked—about 27 million people.
As of 2023, about 65% (56 million) of all adults who smoked had quit. This measure, known as the quit ratio, was lowest (48% to 52%) for:
- People with a GED or no high school education
- People who have lower incomes (less than 100% of the Federal Poverty Level)
- Black people
- People without health insurance or who were insured by Medicaid
Other groups with a high smoking prevalence include:
- American Indian or Alaska Native populations
- People with mental illness
- Sexual and gender diverse people
- Veterans
- People with disabilities
E-cigarettes/vaping devices were the most commonly used tobacco product among US high school students in 2024. After e-cigarettes/vaping devices, nicotine pouches were the next most popular tobacco product in these students followed by cigarettes, cigars, and smokeless tobacco (chewing tobacco, moist snuff, and snus).
Still, e-cigarette use was by far the most popular product.
During and after the pandemic: E-cigarette use declined in young people from a high of 28% in 2019 to just under 8% in 2024 (about 1.21 million students).
After the pandemic, in 2024: E-cigarette use was similar across racial/ethnic groups when previously White students were most likely to use them.
Featured Term: Snus
Rhyming with "loose," this smokeless tobacco product is a small pouch placed between the upper lip and gum. The pouch contains powered tobacco, water, salt, and sometimes a flavor. Nicotine is absorbed through the oral mucosa. The liquids produced are swallowed rather than spit out as they are with snuff products. When finished, the pouch can be thrown away. Snus poses health risks because it contains nicotine, which is addictive. Federal and state laws in the United States prohibit the sale of snus to people younger than 18. This product is popular in Sweden.
Almost 9 out of 10 high school students using a tobacco product in 2023 to 2024 used a flavored one:
- 88% used flavored e-cigarettes (mostly fruit flavored) and nicotine pouches.
- 71% used flavored cigars.
- 42% used menthol cigarettes.
E-cigarette use increased in younger adults (ages 18-24 years) after the pandemic.
- 13% of adults age 18 to 24 used e-cigarettes in 2023 compared to 9% in 2019 before the pandemic.
Obesity levels continued to rise during the pandemic, whereas aerobic physical activity levels and alcohol consumption stayed about the same before, during, and after it.
Excess body weight is associated with an increased risk of developing 13 types of cancer. About 19% of cancer cases in the US can be attributed to a combination of excess body weight, lack of physical activity, unhealthy diet, and consumption of alcohol.
Studies have demonstrated that adults who closely follow the ACS nutrition and physical activity guidelines are less likely to be diagnosed with and die from cancer than those who don’t follow them. Cancer survivors also benefit from healthy eating and active living, which may help improve outcomes and quality of life.
Adults who closely follow the guidelines have a 10% to 20% lower risk of cancer diagnosis and 24% to 30% lower risk of dying from cancer.
Here are some of the review’s key statistics for adults in the US.
Obesity levels continued to climb during August 2021 to August 2023. During that time there were about 40% of adults (age 20 and older) and 21% of children and teens (age 2 to 19) with obesity. Black females have the highest obesity rates at 59% for adults and 39% for children and teens followed by Mexican American females at 51%, from 2017 to March 2020.
In 2022, less than half of adults said they got the recommended levels of aerobic activity and about 30% said they didn’t do any leisure-time physical activity. In 2023, about 1 out of 4 high school students said they met the recommended physical activity levels. These statistics were about the same before the pandemic.
About 6% of adults were classified as heavy drinkers in 2022.
Higher prevalence was observed in:
- White and American Indian or Alaska Native (8%) compared to Black and Hispanic (4%) and Asian (2%) adults.
- People with household incomes at 200% or more of the FPL (7%) compared to those below the poverty level (4%).
These statistics were about the same before the pandemic.
For the study, ACS researchers analyzed national or state-representative data from the National Health Interview Survey (NHIS), the Behavioral Risk Factors Surveillance System (BRFSS), the National Health and Nutrition Examination Survey (NHANES) and the National Immunization Survey-Teen (NIS-TEEN), the National Youth Tobacco Survey (NYTS), and the Youth Risk Behavior Survey (YRBS).
Other ACS researchers contributing to the study include Jessica Star, MA, MPH, Natalia Mazzitelli, MPH, Nigar Nargis, PhD, Farhad Islami, MD, PhD, Rebecca Siegel, MPH, and Robin Yabroff, PhD, MBA.
* The white area, or gap, in the lines for both graphs between 2018 and 2019 delineates a redesign of the National Health Interview Survey (NHIS) in 2019. That redesign prevented a comparison with earlier years of the survey.
# The white area, or gap, for cervical cancer screening in 2003 was due to a lack of information about hysterectomy for that survey year. The gap at the end is because up-to-date cervical cancer screening information was not available in the 2023 NHIS.
American Cancer Society news stories are copyrighted material and are not intended to be used as press releases. For reprint requests, please see our Content Usage Policy.



