What Is Vaginal Cancer?
Vaginal cancer starts in the vagina. There are many different types of vaginal cancer, but the most common is called squamous cell carcinoma. It starts in the lining of the vagina.
The vagina
The vagina starts at the cervix (the lower part of the uterus) and opens at the vulva (the external female genitals). The vagina is usually collapsed with its walls touching each other. The vaginal walls have many folds that help the vagina open and expand during sex or the birth of a baby.
Several different types of cells and tissues are found in the vagina:
- The lining of the vagina has a layer of flat cells called squamous cells. This layer of cells is also called epithelium or epithelial lining because squamous cells are a type of epithelial cell.
- The vaginal wall underneath the epithelium is made up of connective tissue, muscle, lymph vessels, and nerves.
- Glands near the opening of the vagina make mucus to keep the vaginal lining moist.
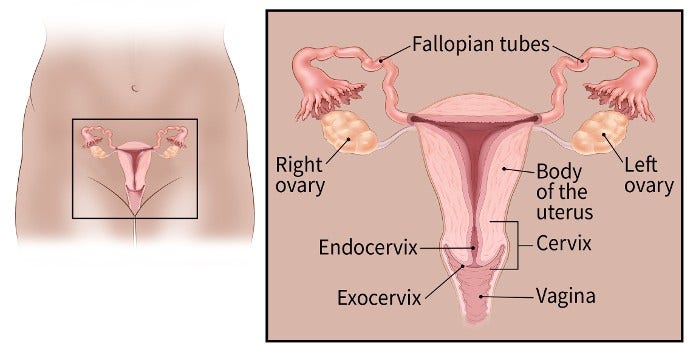
Female reproductive organs
Vaginal pre-cancer (VAIN)
In a pre-cancerous condition, some cells look abnormal. These cell changes are not cancer, but they could become cancer over time. Vaginal intraepithelial neoplasia or VAIN means that the abnormal cells are only found in the innermost surface layer of the vagina, also called the epithelium.
The3 grades of VAIN are based on how deep the abnormal cells are located within the epithelium:
- VAIN 1, also called low-grade VAIN, may go away on its own, but can sometimes lead to cancer if not treated.
- VAIN 2 and VAIN 3, also called high-grade VAIN, are usually treated right away. VAIN 3 is the closest to a true cancer.
When someone has VAIN 3, it means that abnormal cells are found in more than 2/3 of the thickness of vaginal epithelium. If abnormal cells are found within the entire thickness, then it would be called carcinoma in situ.
In the past, the term dysplasia was used instead of VAIN. The types of dysplasia were referred to as mild, moderate, and severe, based on how close it was to a true cancer. This term is used much less now.
VAIN may be found when testing is done to screen for cervical cancer. The HPV test and Pap test (also called a Pap smear) used for cervical cancer screening may also pick up cells from the vaginal lining. This allows some cases of VAIN to be found in women whose vaginal lining is not intentionally scraped. Many women with VAIN may also have a pre-cancer of the cervix (known as cervical intraepithelial neoplasia or CIN). If abnormal cells are found, the next step is a procedure called colposcopy, in which the cervix, the vagina, and at times the vulva are closely examined with a special instrument called a colposcope.
Vaginal cancer and VAIN are more common in women who have had cervical pre-cancer or cancer. In women whose cervix has been removed by surgery to treat cervical cancer or pre-cancer, samples may be taken from the lining of the upper vagina to look for cervical cancer that has come back, and to look for early vaginal cancer or VAIN.
Types of vaginal cancer
Though it's quite rare, there are many types of vaginal cancer. Each type develops from a different type of cell in the vagina.
Squamous cell carcinoma
Most cases of vaginal cancer are squamous cell carcinomas. These cancers start in the squamous cells that make up the epithelial lining of the vagina. They're most common in the upper part of the vagina near the cervix. If not treated, over time, they can grow deeper into and through the vaginal wall and spread to nearby tissues. They can also spread to other parts of the body, most often the lungs, but also the liver and bones.
Squamous cell cancers of the vagina often develop slowly. First, some of the normal cells of the vagina get pre-cancerous changes (VAIN). Then some of the pre-cancer cells turn into cancer cells. This process can take many years.
Adenocarcinoma
Cancers that begin in gland cells are called adenocarcinomas. About 1 of every 10 cases of vaginal cancer are adenocarcinomas.
The most common type of vaginal adenocarcinoma is found in women older than 50. Another type, called clear cell adenocarcinoma, is more common in young women who were exposed to diethylstilbestrol (DES) in utero (when they were in their mother’s womb). (See Risk Factors for Vaginal Cancer for more information on DES and clear cell carcinoma.)
Very rare vaginal cancers
Melanoma
Melanomas start in pigment-producing cells that give skin its color. These cancers usually are found on sun-exposed areas of the skin but also can form in the vagina or other internal organs. About 3 of every 100 cases of vaginal cancer are melanomas.
Melanoma tends to affect the lower or outer portion of the vagina. The tumors vary greatly in size, color, and growth pattern. Although vaginal melanomas can be blue, black, or brown, many are non-pigmented. More information about melanoma can be found in Melanoma Skin Cancer.
Sarcoma
Sarcomas are cancers that start in the cells of bones, muscles, or connective tissue. Fewer than 3 of every 100 cases of vaginal cancer are sarcomas. These cancers form deep in the wall of the vagina, not on its surface.
There are several types of vaginal sarcomas. Rhabdomyosarcoma is the most common type of sarcoma that affects the vagina. It’s most often found in children and is rare in adults. A sarcoma called leiomyosarcoma is seen more often in adults. It tends to occur in women older than 50.
Cancers that spread to the vagina
Cancers that start in the vagina are much less common than cancers that start in other organs (such as the cervix, uterus, rectum, or bladder) and then spread to the vagina. These cancers are named after the place they started.
If a cancer is growing in both the cervix and vagina, it is considered a cervical cancer. If the cancer involves both the vulva and the vagina, it’s considered a vulvar cancer cancer.
- Written by
- References

Developed by the American Cancer Society medical and editorial content team with medical review and contribution by the American Society of Clinical Oncology (ASCO).
Adams TS, Rogers LJ, Cuello MA. Cancer of the vagina: 2021 update. Int J Gynaecol Obstet. 2021 Oct;155 Suppl 1(Suppl 1):19-27. doi: 10.1002/ijgo.13867. PMID: 34669198; PMCID: PMC9298013.
Cao D, Wu D, Xu Y. Vaginal intraepithelial neoplasia in patients after total hysterectomy. Curr Probl Cancer. 2021 Jun;45(3):100687. doi: 10.1016/j.currproblcancer.2020.100687. Epub 2020 Dec 4. PMID: 33309077.
Kesic V, Carcopino X, Preti M, Vieira-Baptista P, Bevilacqua F, Bornstein J, Chargari C, et al. The European Society of Gynaecological Oncology (ESGO), the International Society for the Study of Vulvovaginal Disease (ISSVD), the European College for the Study of Vulval Disease (ECSVD), and the European Federation for Colposcopy (EFC) consensus statement on the management of vaginal intraepithelial neoplasia. Int J Gynecol Cancer. 2023 Apr 3;33(4):446-461. doi: 10.1136/ijgc-2022-004213. PMID: 36958755; PMCID: PMC10086489.
National Cancer Institute. Vaginal Cancer Treatment (PDQ®)–Health Professional Version. February 16, 2024. Accessed at www.cancer.gov/types/vaginal/hp/vaginal-treatment-pdq on August 12, 2024.
Last Revised: September 23, 2024
American Cancer Society medical information is copyrighted material. For reprint requests, please see our Content Usage Policy.
American Cancer Society Emails
Sign up to stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society.


