Chemotherapy for Liver Cancer
Chemotherapy (chemo) is treatment with certain kinds of drugs that destroy cancer cells.
When is chemotherapy used for liver cancer?
Chemo may be an option for people whose liver cancer can’t be treated with surgery or other local therapies such as ablation or embolization.
At one time, chemo was often the first treatment for more advanced liver cancers. But newer types of treatment, such as immunotherapy and targeted therapy drugs, are more likely to be helpful, so these drugs are now typically used first instead.
Chemo might still be an option for people who have already had these treatments or can’t get them for some reason.
Hepatic artery infusion of chemo (described below) might also be an option for some people whose cancer can’t be removed completely.
Which chemotherapy drugs are used for liver cancer?
Chemo drugs that might be used to treat liver cancer include:
- Gemcitabine
- Oxaliplatin
- Cisplatin
- Doxorubicin (or pegylated liposomal doxorubicin)
- 5-fluorouracil (5-FU)
- Capecitabine
- Mitoxantrone
Sometimes, combinations of 2 or 3 of these drugs are used, if a person can tolerate it. For example:
- GEMOX (gemcitabine plus oxaliplatin) might be an option for people who are healthy enough tolerate more than one drug.
- FOLFOX (5-FU, oxaliplatin and leucovorin) might be another option for some people.
How is chemotherapy given for liver cancer?
Chemo can be given in different ways.
Systemic chemotherapy
In this approach, drugs are given into a vein (IV) or taken by mouth. These drugs enter the blood and reach almost all areas of the body, which can make this treatment useful for cancers that have spread to other parts of the body.
For some people, IV chemo might be given through a slightly larger and sturdier tube known as a central venous catheter (CVC), central venous access device (CVAD), or central line. This device is put in place with a minor surgical procedure. It stays in the body and can be used to put medicines, blood products, nutrients, or fluids right into your blood. It can also be used to take out blood for testing.
Doctors give chemo in cycles, with each period of treatment followed by a rest period to give you time to recover from the effects of the medicine. Cycles are most often 2 or 3 weeks long. The schedule varies depending on the medicines used. For example, with some medicines, the chemo is given only on the first day of the cycle. With others, it is given for a few days in a row, or once a week.
The length of chemo treatment will be based on how well it is working and what side effects you have.
Hepatic artery infusion
During hepatic artery infusion (HAI), chemo is given directly into the hepatic artery, a large artery that feeds into the liver. This focuses the chemo on the cancer cells in the liver.
The drug enters the liver and affects the cancer cells, while the healthy liver cells break down most of the drug before it can reach the rest of the body. This method gets a higher dose of chemo to the tumor than systemic chemo while limiting side effects in the rest of the body.
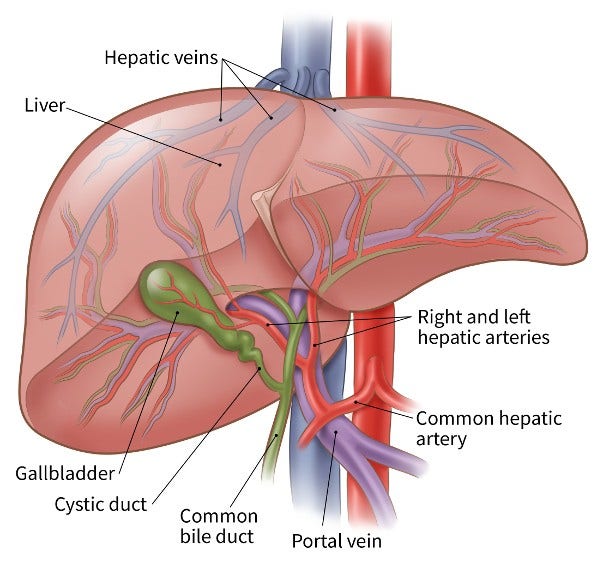
Hepatic artery infusion is slightly different from chemoembolization because surgery is needed to put an infusion pump under the skin of the abdomen (belly). The pump is attached to a catheter that connects to the hepatic artery. This is done while a person is under general anesthesia (in a deep sleep so they won’t feel pain). The chemo is then injected with a needle through the skin into the pump's reservoir, and it is released slowly and steadily into the hepatic artery.
HAI may be used for people with very large liver cancers that cannot be removed with surgery or cannot be treated entirely with trans-arterial chemoembolization (TACE). But many people with liver cancer may not be able to tolerate surgery to insert the pump and catheter, and not all centers offer this type of treatment.
Possible side effects of chemotherapy for liver cancer
Chemo drugs attack cells in the body that are dividing quickly, which can lead to side effects.
The side effects depend on the type and dose of chemo drugs, as well as how long they are given. Common side effects include:
- Hair loss
- Mouth sores
- Loss of appetite
- Nausea and vomiting
- Diarrhea
- Increased chance of infections (from having too few white blood cells)
- Easy bruising or bleeding (from having too few blood platelets)
- Feeling tired (from having too few red blood cells)
These side effects usually go away after treatment is finished. There are often ways to lessen them. For example, drugs can be given to help prevent or reduce nausea and vomiting. Be sure to ask your cancer care team about medicines to help reduce side effects.
Along with the possible side effects above, some drugs may have their own specific side effects. Ask your cancer care team what you can expect.
Be sure to tell your health care team about any side effects that you notice while getting chemo so that you can be treated right away. In some cases, the doses of the chemo drugs may need to be reduced, or treatment may need to be delayed or stopped to keep the side effects from getting worse.
More information about chemotherapy
For more general information about how chemotherapy is used to treat cancer, see Chemotherapy.
To learn about some of the side effects listed here and how to manage them, see Managing Cancer-related Side Effects.
- Written by
- References

Developed by the American Cancer Society medical and editorial content team with medical review and contribution by the American Society of Clinical Oncology (ASCO).
Abdalla EK, Stuart KE, Singal AG. Overview of treatment approaches for hepatocellular carcinoma. UpToDate. 2024. Accessed at https://www.uptodate.com/contents/overview-of-treatment-approaches-for-hepatocellular-carcinoma on December 9, 2024.
Fong Y, Covey AM, Feng M, Daneng L. Ch 36: Cancer of the Liver. In: DeVita VT, Lawrence TS, Rosenberg SA, eds. DeVita, Hellman, and Rosenberg's Cancer: Principles & Practice of Oncology. 12th ed. Philadelphia, PA: Wolters Kluwer; 2023.
National Cancer Institute. Primary Liver Cancer Treatment (PDQ®)–Health Professional Version. Accessed at https://www.cancer.gov/types/liver/hp/adult-liver-treatment-pdq on September 16, 2024.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Hepatocellular Carcinoma. Version 3.2024. Accessed at https://www.nccn.org/ on December 9, 2024.
Si T, Huang Z, Khorsandi SE, Ma Y, Heaton N. Hepatic arterial infusion chemotherapy versus transarterial chemoembolization for unresectable hepatocellular carcinoma: A systematic review with meta-analysis. Front Bioeng Biotechnol. 2022:10:1010824.
Stuart KE. Systemic treatment for advanced hepatocellular carcinoma. 2024. Accessed at https://www.uptodate.com/contents/systemic-treatment-for-advanced-hepatocellular-carcinoma on December 9, 2024.
Last Revised: February 11, 2025
American Cancer Society medical information is copyrighted material. For reprint requests, please see our Content Usage Policy.
American Cancer Society Emails
Sign up to stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society.


