Your Colon or Rectal Pathology Report: Early Adenocarcinoma (Cancer) in a Polyp
Biopsy samples collected from your colon or rectum are studied by a doctor with special training, called a pathologist. After testing the samples, the pathologist creates a report on what was found. Your doctor can use this report to help manage your care.
The information here is meant to help you understand some of the medical terms you might see in your pathology report after your colon or rectum is biopsied.
(If you have colon or rectal cancer and have surgery to treat it, a separate pathology report will be created after testing the part of the colon or rectum that was removed. That report might have some of the same information below, as well as other information.)
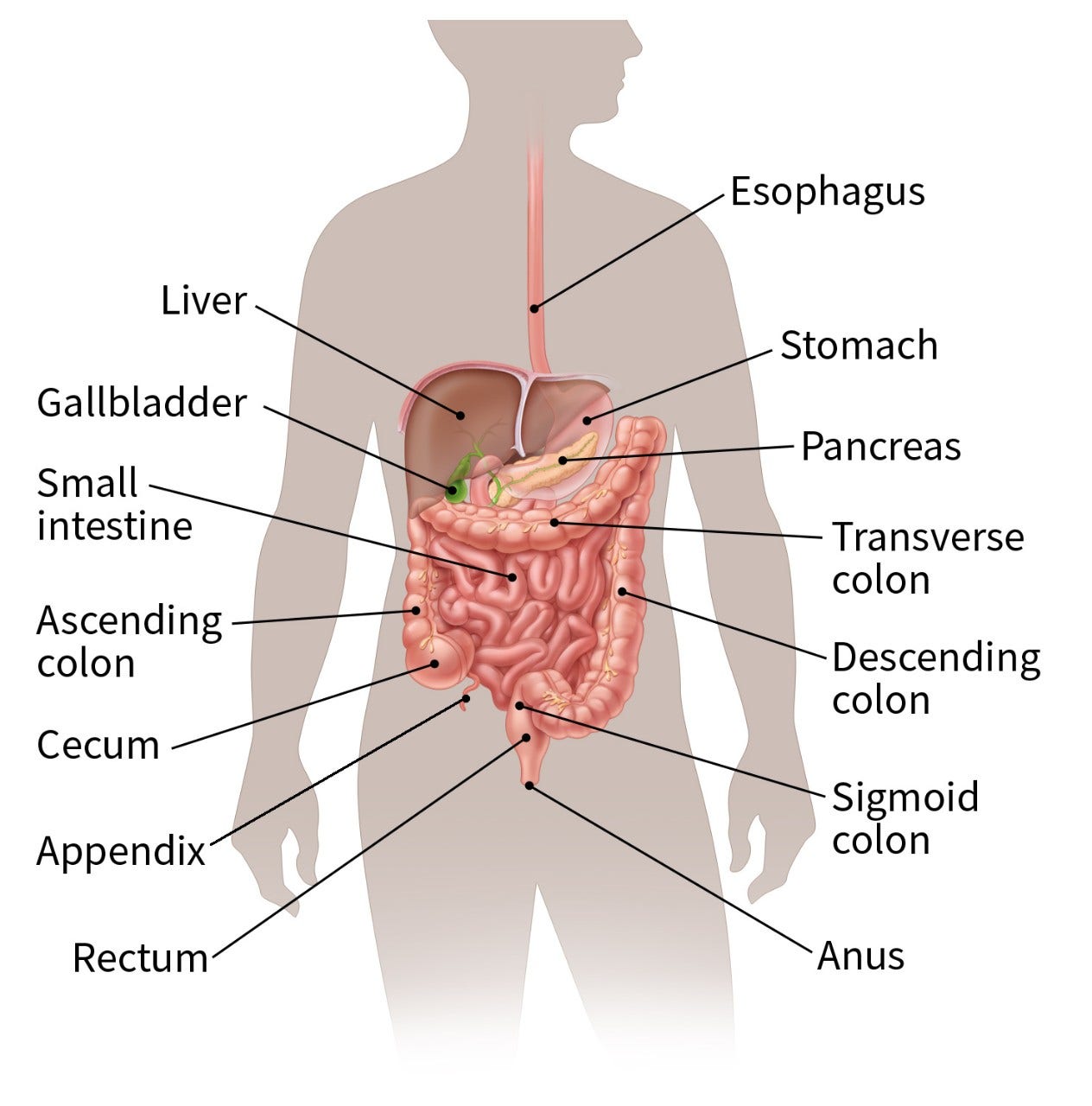
Parts of the colon and rectum
The colon and rectum make up the large intestine (or large bowel), which is part of the digestive system. The cecum is the beginning of the colon, where the small intestine empties into the large intestine. The ascending colon, transverse colon, descending colon, and sigmoid colon are the parts of the colon after the cecum. The colon ends at the rectum, where waste (stool) is stored until it leaves the body through the anus.
Colon or rectal polyps
A polyp is a projection (growth) from the inner lining into the lumen (hollow center) of the colon or rectum. Colon and rectal polyps are common. Most polyps are benign (non-cancerous) growths, but cancer can start in some types of polyps.
Adenomas
An adenoma (adenomatous polyp) is a type of polyp made up of tissue that looks much like the normal lining of your colon or rectum, although it is different in some important ways when looked at with a microscope. Sometimes, cancer can start in an adenoma.
There are different types of adenomas, which are often described based on their growth patterns when seen under a microscope. Types of adenomas include:
- Tubular adenoma
- Tubulovillous adenoma
- Villous adenoma
- Sessile serrated adenoma (sessile serrated polyp)
- Traditional serrated adenoma
To learn more about adenoma types, see Your Colon or Rectal Pathology Report: Polyps.
The type of adenoma affects how likely it is to contain cancer cells. But if cancer develops in an adenoma, the type of the adenoma is not as important in terms of treatment as other factors (see below).
Types of cancer that might be found in a colon or rectal polyp
Carcinoma
Carcinoma is the general medical term for a cancer that starts in the cells that line the insides of organs such as the colon or rectum. Most cancers that start in the colon or rectum are carcinomas (specifically adenocarcinomas – see below).
Adenocarcinoma of the colon (or rectum)
Adenocarcinoma is a type of cancer that starts in the gland cells that make mucus to lubricate and protect the inside of the colon and rectum. This is the most common type of colon cancer. Other types of tumors or cancers can also start in the colon or rectum, although these are much less common than adenocarcinomas.
Very early colon and rectal cancers
Sometimes on a biopsy, cells that look like cancer cells are found only in the top layers of the polyp or of the colon/rectal lining (called the mucosa). This might be described with one of these terms:
- High-grade dysplasia
- Intramucosal carcinoma
- Carcinoma in situ (CIS)
- Carcinoma in the lamina propria
This type of early cancer does not yet have the ability to spread to other parts of the body, so it may be called a pre-cancer.
While an adenoma with one of these conditions still needs to be removed completely, this is not the same as having a true colon or rectal cancer, since it cannot spread. Still, people who have one of these findings in an adenoma will likely need colonoscopies more often in the future to look for more polyps.
Invasive or infiltrating adenocarcinoma
If an adenocarcinoma is described as infiltrating or invasive, it means the cancer cells have grown deeper than the top layers of the polyp or colon/rectal lining (mucosa), so this is a true cancer (and not a pre-cancer). At this point, the cancer cells can grow through the wall of the colon or rectum and into nearby structures, or they may spread to nearby lymph nodes and other parts of the body.
But being infiltrative or invasive doesn’t necessarily mean that the cancer has grown deeply into the wall of the colon or rectum. A biopsy only samples a small part of a tumor, so it can’t always show how deeply the tumor has invaded into the wall. To know this, the pathologist needs to see the entire tumor (removed during surgery).
Other information if colon or rectal cancer is found in a polyp
If colon or rectal carcinoma (cancer) is found, the pathologist might provide other information in the pathology report.
Cancer grade (differentiation)
If cancer is found, it will likely be assigned a grade, based on how abnormal the cancer cells look under a microscope. Colon or rectal cancer can have 3 grades:
- Well differentiated (low grade)
- Moderately differentiated (intermediate grade)
- Poorly differentiated (high grade)
Sometimes, it might just be described as either well/moderately differentiated (low grade) or poorly differentiated (high grade).
Poorly differentiated (high-grade) cancers tend to grow and spread more quickly than well or moderately differentiated cancers.
If a polyp contains poorly differentiated adenocarcinoma (cancer), you may need to have surgery to remove part of your colon or rectum to make sure that the tumor has not grown outside the colon or rectum. Talk to your doctor to see what treatment options might be best for you.
Vascular, lymphatic, or lymphovascular (angiolymphatic) invasion
These terms mean that the cancer has grown into the small blood vessels and/or lymph vessels (lymphatics) of the colon or rectum, so there is a higher chance that it could have spread outside the colon or rectum. However, this doesn’t mean that your cancer has spread.
Still, when vascular, lymphatic, or lymphovascular invasion is present, you may need surgery to remove part of your colon or rectum to make sure the tumor has not grown outside the colon or rectum. Talk to your doctor to see what treatment options might be best for you.
If a polyp with invasive adenocarcinoma was not entirely removed…
If a polyp (adenoma) with invasive adenocarcinoma wasn’t removed completely during a colonoscopy, you’ll most likely need another procedure to remove it. While this is most often an operation done by a surgeon, your doctor will discuss what treatment options are best for you.
If invasive adenocarcinoma in a polyp was entirely removed…
If a polyp (adenoma) with invasive adenocarcinoma was removed completely, you might not need any further treatment (like surgery), as long as the cancer was not poorly differentiated (see above) and did not have vascular, lymphatic, or lymphovascular invasion (see above). Talk to your doctor about what treatment options might be best for you.
If polyps were also found in other parts of the colon or rectum…
Having more than one colon or rectal polyp is not uncommon. There are different types of polyps, some of which are more concerning than others.
For example, hyperplastic polyps are typically benign (not cancer or pre-cancer) and are not a cause for concern. But the different types of adenomatous polyps (adenomas), which are discussed above, are more of a concern because they might turn into cancer. (To learn more, see Your Colon or Rectal Pathology Report: Polyps.)
Still, if polyps are present in addition to cancer elsewhere in the colon, they don’t usually affect the treatment or follow-up of the cancer.
- Written by

The American Cancer Society medical and editorial content team
Our team is made up of doctors and oncology certified nurses with deep knowledge of cancer care as well as editors and translators with extensive experience in medical writing.
Last Revised: July 7, 2023
American Cancer Society medical information is copyrighted material. For reprint requests, please see our Content Usage Policy.
American Cancer Society Emails
Sign up to stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society.


