Surgery for Prostate Cancer
Surgery is a common choice to try to cure prostate cancer if it is not thought to have spread outside the prostate gland.
Radical prostatectomy
The main type of surgery for prostate cancer is a radical prostatectomy. In this operation, the surgeon (urologist) removes the entire prostate gland plus some of the tissue around it, including the seminal vesicles. Sometimes nearby lymph nodes are removed as well.
There are 2 main ways a surgeon can do a radical prostatectomy:
- In an open prostatectomy, the surgeon operates through a single long skin incision (cut) to remove the prostate and nearby tissues.
- In a laparoscopic prostatectomy, the surgeon makes several smaller incisions and uses long, thin surgical tools to remove the prostate and nearby tissues. Most often, the surgeon sits at a control panel to precisely move robotic arms that hold the tools (known as a robot-assisted prostatectomy or robotic prostatectomy). The operation can also be done with the surgeon holding the tools directly, although this is less common.
With either type of operation, if there’s a reasonable chance the cancer might have spread to nearby lymph nodes (based on your PSA level, prostate biopsy results, and other factors), the surgeon may first remove some of these lymph nodes (known as a pelvic lymph node dissection). The nodes are sent to the lab to be looked at right away for cancer cells. If cancer cells are found in any of the nodes, the surgeon might not continue with the surgery. This is because it’s unlikely that the cancer can be cured with surgery, and removing the prostate could lead to serious side effects.
Open prostatectomy
This type of surgery is done less often than in the past, as robotic prostatectomy (see below) has become more common. There are 2 main approaches for an open prostatectomy.
Radical retropubic prostatectomy
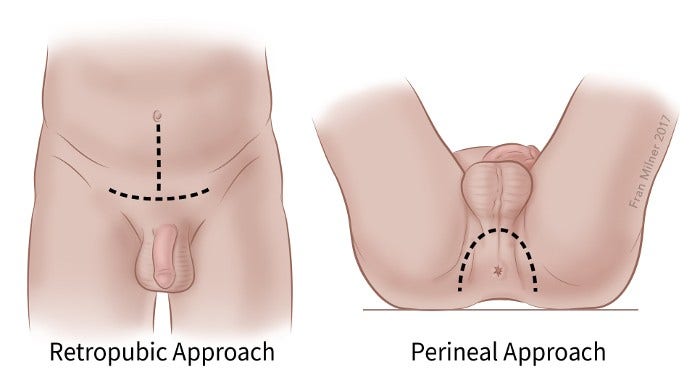
For this operation, the surgeon makes an incision (cut) in your lower abdomen, from the belly button down to the pubic bone, as shown in the picture below. You will either be under general anesthesia (asleep) or be given spinal or epidural anesthesia (numbing the lower half of the body) along with sedation during the surgery.
After the prostate and nearby structures have been removed, and while you are still under anesthesia, a catheter (thin, flexible tube) will be put in your penis to help drain your bladder. The catheter will usually stay in place for 1 to 2 weeks while you heal. You will be able to urinate on your own after the catheter is removed.
You will probably stay in the hospital for a few days after the surgery, and your activities will be limited for several weeks.
Radical perineal prostatectomy
In this open operation, the surgeon makes the cut (incision) in the skin between the anus and scrotum (the perineum), as shown in the picture above.
This approach is used less often because it’s more likely to lead to erection problems and because the nearby lymph nodes can’t be removed during the operation. But it is often a shorter operation, and it may result in less pain and an easier recovery than a retropubic prostatectomy.
This approach might be an option if you aren’t concerned about erections and if you don’t need lymph nodes removed. It also might be used if you have other medical conditions that might make retropubic surgery difficult for you. It is just as likely to cure prostate cancer as the retropubic approach if done correctly.
After the surgery, and while you are still under anesthesia, a catheter will be put in your penis to help drain your bladder. The catheter usually stays in place for 1 to 2 weeks while you are healing. You will be able to urinate on your own after the catheter is removed.
You will probably stay in the hospital for a few days after the surgery, and your activities will be limited for several weeks.
Laparoscopic prostatectomy (including robotic prostatectomy)
Laparoscopic surgery is done through several small incisions in the abdomen, rather than one large incision. The surgeon inserts a laparoscope, which is a long, thin tube with a light and tiny video camera on the end, through one of the openings so they can see inside the body. Long, thin surgery instruments are then inserted through the other incisions to perform the operation.
This approach to prostatectomy (particularly robotic prostatectomy) has become much more common in recent years.
Laparoscopic radical prostatectomy
For a laparoscopic radical prostatectomy (LRP), the surgeon holds the handles of the long instruments directly to maneuver them inside the belly and remove the prostate. This approach is not used as often as robotic prostatectomy.
Robotic prostatectomy
This approach, also known as robotic-assisted laparoscopic radical prostatectomy or robot-assisted prostatectomy, is the most common way prostatectomy is done in the United States.
This operation is done using a robotic system. The surgeon sits at a control panel in the operating room and moves robotic arms to operate through several small incisions, usually in the patient’s abdomen (although it can also be done with a perineal approach). The robotic system helps the surgeon move the instruments more precisely than if they were holding the laparoscopic tools directly in their hands.
Robotic versus open radical prostatectomy: Things you should know
Robotic prostatectomy is the most common surgery to treat prostate cancer in the United States (and some other countries). That is largely because this operation has some short-term advantages over open radical prostatectomy. For example, it usually results in:
- Less blood loss during the operation
- Less pain after the operation
- A shorter hospital stay
- A quicker recovery time
- Less time the urinary catheter needs to stay in place
- A lower risk of some rare but potentially serious side effects
However, the results of robotic and open prostatectomy seem to be about the same when it comes to the long-term side effects that many men are most concerned about, including erection problems and trouble holding urine (incontinence). (These are described below.)
There also doesn’t appear to be much difference between robotic and open prostatectomy when it comes to long-term outcomes. That is, studies haven’t shown that either approach is clearly better than the other when it comes to how likely the cancer is to return after surgery or how likely a man is to die from prostate cancer. Both approaches generally result in good outcomes when done by experienced surgeons.
In some instances, there might be clear reasons to favor one approach over the other.
But no matter which prostatectomy approach you choose, the biggest factor in the success of your surgery is likely to be the experience and skill of your surgeon. Because of this, it’s very important to find an experienced surgeon whom you’re comfortable with and whom you can trust.
Risks of prostatectomy
The risks with any type of radical prostatectomy are much like those of any major surgery. Problems during or shortly after the operation can include:
- Reactions to anesthesia
- Bleeding from the surgery
- Blood clots in the legs or lungs
- Damage to nearby organs
- Infections at the surgery site
Rarely, part of the intestine might be injured during surgery, which could lead to infections in the abdomen and might require more surgery to fix. Injuries to the intestines are more common with laparoscopic and robotic surgeries than with the open approach.
If lymph nodes are removed, a collection of lymph fluid (called a lymphocele) can form and may need to be drained.
Your risks depend, in part, on your overall health, your age, and the skill of your surgical team.
Side effects of prostatectomy
The major possible side effects of radical prostatectomy are:
- Urinary incontinence (being unable to control urine)
- Erectile dysfunction (problems getting or keeping erections)
These side effects can also occur with some other forms of prostate cancer treatment.
Other side effects are also possible (see below).
Urinary incontinence
You may not be able to control your urine, or you may have leakage or dribbling after your surgery. Being incontinent can affect you not only physically, but also emotionally and socially. These are the major types of incontinence:
- Men with stress incontinence might leak urine when they cough, laugh, sneeze, or exercise. Stress incontinence is the most common type after prostate surgery. It’s usually caused by problems with the valve that keeps urine in the bladder (the bladder sphincter). Prostate cancer treatments can damage this valve or the nerves that keep the valve working.
- Men with overflow incontinence have trouble emptying their bladder. They take a long time to urinate and have a dribbling stream with little force. Overflow incontinence is usually caused by blockage or narrowing of the bladder outlet by scar tissue.
- Men with urge incontinence have a sudden need to urinate. This happens when the bladder becomes too sensitive to stretching as it fills with urine.
- Rarely after surgery, men lose all ability to control their urine. This is called continuous incontinence.
After surgery for prostate cancer, bladder control usually improves slowly over several weeks or months. But doctors can’t predict for sure how any man will be affected. In general, older men tend to have more incontinence problems than younger men. Large cancer centers, where prostate surgery is done often and surgeons have a lot of experience, generally report fewer problems with incontinence.
Incontinence can be treated. Even if your incontinence can’t be corrected completely, it can still be helped. To learn about managing and living with incontinence, see Bladder and Bowel Incontinence.
Erectile dysfunction (impotence)
This means you can’t get an erection sufficient for sexual penetration.
Erections are controlled by 2 tiny bundles of nerves that run along either side of the prostate. If you can have erections before surgery, the surgeon will try not to injure these nerves during the prostatectomy. This is known as a nerve-sparing approach. But if the cancer is growing into or very close to the nerves, the surgeon will need to remove them.
If both nerves are removed, you won’t be able to have spontaneous erections, but you might still be able to have erections using some of the aids described below. If the nerves on only one side are removed, you might still have erections, but the chance is lower than if neither were removed. If neither nerve bundle is removed, you might have normal erections at some point after surgery.
Your ability to have an erection after surgery depends on your age, your ability to get an erection before the operation, and whether the nerves were cut. Most men will probably have at least some loss of ability to have an erection, but the younger you are, the less likely you are to be seriously affected.
Surgeons who do many prostatectomies tend to report lower rates of erection problems among their patients than those who do the surgery less often. A wide range of rates have been reported in the medical literature, but each man’s situation is different, so the best way to get an idea of your chances for recovering erections is to ask about your doctor’s success rates and what the outcome is likely to be in your case.
If your ability to have erections does return after surgery, it often returns slowly. In fact, it can take from a few months to 2 or more years. During the first few months, you will probably not be able to have a spontaneous erection, so you may need to use medicines or other treatments.
Many doctors feel that regaining potency is helped along by trying to get an erection as soon as possible once the body has had a chance to heal (usually several weeks after the operation). Some doctors call this penile rehabilitation. Medicines (see below) may be helpful at this time, although it’s not clear if they work better if taken daily or just on an as-needed basis. Be sure to talk to your doctor about your situation.
There are several options for treating erectile dysfunction:
- Phosphodiesterase-5 (PDE5) inhibitors, such as sildenafil (Viagra), vardenafil (Levitra), tadalafil (Cialis), and avanafil (Stendra), are pills that can help with erections. These drugs won’t work if both nerves that control erections have been damaged or removed. Common side effects of these drugs include headache, flushing (skin becoming red and feeling warm), upset stomach, light sensitivity, and runny or stuffy nose. Rarely, these drugs can cause vision problems, possibly even blindness. Some other drugs such as nitrates, which are used to treat heart disease, can cause problems if you are taking a PDE5 inhibitor, so be sure your doctor knows what medicines you take.
- Alprostadil is a man-made version of prostaglandin E1, a substance naturally made in the body that can produce erections. It can be injected almost painlessly into the base of the penis 5 to 10 minutes before intercourse or placed into the tip of the penis as a suppository. You can even increase the dosage to prolong the erection. You might have side effects, such as pain, dizziness, and prolonged erection, but they are not usually serious.
- Vacuum devices are another option to create an erection. These are clear, plastic tubes connected to pumps that are placed over the penis. The pump sucks the air out of the tube, which draws blood into the penis to produce an erection. After the device is removed, the erection is maintained by placing an elastic ring around the base of the penis, which keeps the blood from draining out. The ring is then removed after sex.
- Penile implants might restore your ability to have erections if other methods don’t help. An operation is needed to put them inside the penis. There are several types of penile implants, including those using silicone rods or inflatable devices.
For more on coping with erection problems and other sexuality issues, see Sexual Side Effects.
Changes in orgasm
After surgery, the sensation of orgasm should still be pleasurable, but there is no ejaculation of semen – the orgasm is “dry.” This is because the glands that made most of the fluid for semen (the seminal vesicles and prostate) were removed during the prostatectomy, and the pathways used by sperm (the vas deferens) were cut. In some men, orgasms might become less intense. Less often, men report pain with orgasm.
Loss of fertility
During a radical prostatectomy, the surgeon cuts the vas deferens, which are the pathways between the testicles (where sperm are made) and the urethra (through which sperm leave the body). Your testicles will still make sperm, but they can’t leave the body as a part of the ejaculate. This means that a man can no longer father a child the natural way.
Often, this is not an issue, as men with prostate cancer tend to be older. But if it is a concern for you, you might want to ask your doctor about “banking” your sperm before the operation. To learn more, see Fertility Problems.
Lymphedema
This is a rare but possible complication of removing many of the lymph nodes around the prostate. Lymph nodes normally provide a way for fluid to return to the heart from all areas of the body. When nodes are removed, fluid can collect in the legs or genital region over time, causing swelling and pain.
Lymphedema can usually be treated with physical therapy, although it may not go away completely. You can learn more on our lymphedema page.
Change in penis length
A possible effect of surgery is a small decrease in penis length. This can result from a shortening of the urethra when a portion of it is removed along with the prostate.
Inguinal hernia
A prostatectomy increases a man’s chances of developing an inguinal (groin) hernia in the future.
Transurethral resection of the prostate (TURP)
This operation is more often used to treat men with non-cancerous enlargement of the prostate called benign prostatic hyperplasia (BPH). But it is also sometimes used in men with advanced prostate cancer to help relieve symptoms, such as trouble urinating. (It is not used to try to cure the cancer.)
During this operation, the surgeon removes the inner part of the prostate gland that surrounds the urethra (the tube through which urine leaves the bladder). The skin is not cut with this surgery. An instrument called a resectoscope is passed through the tip of the penis and into the urethra to the level of the prostate. Once it’s in place, either electricity is passed through a wire to heat it or a laser is used to cut or vaporize the tissue.
This operation is done with either spinal anesthesia (which numbs the lower half of your body) or general anesthesia (where you are in a deep sleep), and it usually takes about an hour.
After surgery, a catheter (thin, flexible tube) is inserted through the penis and into the bladder. It remains in place for about a day to help urine drain while the prostate heals. You can usually leave the hospital after 1 to 2 days and return to normal activities in 1 to 2 weeks.
You will probably have some blood in your urine after surgery.
Other possible side effects from TURP include infection and any risks that come with the type of anesthesia used.
Orchiectomy (castration)
In this operation, the surgeon removes the testicles, where most of the androgens (male hormones) are made. Although this is a type of surgery, its main effect is as a form of hormone therapy. To learn more about this operation, see Hormone Therapy for Prostate Cancer.
More information about surgery
For more general information about surgery as a treatment for cancer, see Cancer Surgery.
To learn about some of the side effects listed here and how to manage them, see Managing Cancer-related Side Effects.
- Written by
- References

The American Cancer Society medical and editorial content team
Our team is made up of doctors and oncology certified nurses with deep knowledge of cancer care as well as editors and translators with extensive experience in medical writing.
Barnas JL, Pierpaoli S, Ladd P, et al. The prevalence and nature of orgasmic dysfunction after radical prostatectomy. BJU Int. 2004;94:603-605.
Bekelman JE, Rumble RB, Chen RC, et al. Clinically Localized Prostate Cancer: ASCO Clinical Practice Guideline Endorsement of an American Urological Association/American Society for Radiation Oncology/Society of Urologic Oncology Guideline. J Clin Oncol. 2018; 32: 3251-3258.
Chang P, Wagner AA, Regan MM, et al. Prospective multicenter comparison of open and robotic radical prostatectomy: The PROST-QA/RP2 Consortium. J Urol. 2022;207(1):127-136.
Klein EA. Radical prostatectomy for localized prostate cancer. UpToDate. 2023. Accessed at https://www.uptodate.com/contents/radical-prostatectomy-for-localized-prostate-cancer on August 6, 2023.
National Cancer Institute. Physician Data Query (PDQ). Prostate Cancer Treatment – Health Professional Version. 2023. Accessed at https://www.cancer.gov/types/prostate/hp/prostate-treatment-pdq on August 5, 2023.
National Comprehensive Cancer Network (NCCN). Practice Guidelines in Oncology: Prostate Cancer. Version 2.2023. Accessed at https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf on August 5, 2023.
Nelson WG, Antonarakis ES, Carter HB, et al. Chapter 81: Prostate Cancer. In: Niederhuber JE, Armitage JO, Doroshow JH, Kastan MB, Tepper JE, eds. Abeloff’s Clinical Oncology. 6th ed. Philadelphia, Pa: Elsevier; 2020.
Quinlan DM, Epstein JI, Carter BS, Walsh PC. Sexual function following radical prostatectomy: Influence of preservation of neurovascular bundles. J Urol. 1991;145:998-1002.
Savoie M, Kim SS, Soloway MS. A prospective study measuring penile length in men treated with radical prostatectomy for prostate cancer. J Urol. 2003;169:1462-1464.
Sun M, Lughezzani G, Alasker A, et al. Comparative study of inguinal hernia repair after radical prostatectomy, prostate biopsy, transurethral resection of the prostate or pelvic lymph node dissection. J Urol. 2010;183:970-975.
Zelefsky MJ, Morris MJ, and Eastham JA. Chapter 70: Cancer of the Prostate. In: DeVita VT, Lawrence TS, Rosenberg SA, eds. DeVita, Hellman, and Rosenberg’s Cancer: Principles and Practice of Oncology. 11th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2019.
Last Revised: November 22, 2023
American Cancer Society medical information is copyrighted material. For reprint requests, please see our Content Usage Policy.
American Cancer Society Emails
Sign up to stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society.


