1 of Every 4 Global Cancer Deaths Are Caused by Tobacco Use
ACS researchers say that lung cancer can be largely prevented through effective tobacco control policies and regulations across the globe.
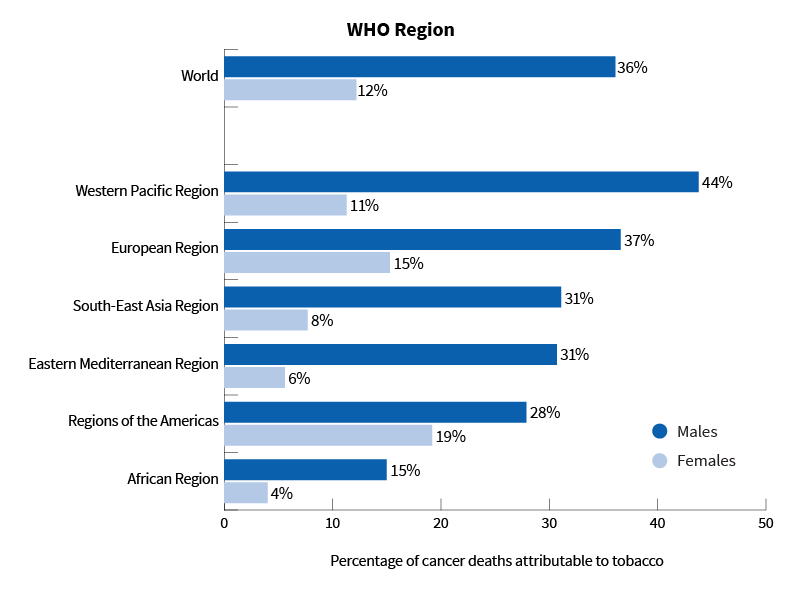
Deaths from Cancer Caused from Using Tobacco, Worldwide in 2019
This graphic shows that:
- Around the world, 3x as many men (36%) died from a tobacco-related cancer compared to women (12%) who died.
- The highest percentage (44%) of men (dark blue bar) who died from a tobacco-related cancer were in the Western Pacific Region of the World Health Organization (WHO). This region includes China, Japan, Australia, and New Zealand.
- The highest percentage (19%) of women (light blue bar) who died from a cancer caused by smoking were in the Americas Region of the WHO. This region includes North America, Central America, South America, Cuba, and the Caribbean Islands.
- The fewest deaths from a tobacco-related type of cancer for both men (15%) and women (4%) in 2019 was in the WHO African Region. That region includes all African countries, except Morocco, Tunesia, Libya, Egypt, Sudan, and Somalia.
Tobacco use remains the main cause of lung cancer, and the disease can largely be prevented through effective tobacco control policies and regulations.
Aggressive tobacco marketing, coupled with inadequate governmental policies, contributes to the increases in smoking prevalence.
In 2007, the World Health Organization (WHO) developed the Framework Convention on Tobacco Control, which includes guidelines to help nations reduce the demand for tobacco products by implementing and managing efficient tobacco control.
One of the most effective interventions to reduce tobacco use is to increase the average tobacco tax. Yet tobacco taxation has been the slowest measure to progress. Only the European region reaches tax benchmark suggested by the WHO—taxes that equal at least 75% of the cigarette retail price.
In Europe alone, implementing the highest level of tobacco control policies could prevent an estimated 1.65 million cases of lung cancer over a 20-year period. All levels of government need to work together for successful tobacco control.
American Cancer Society news stories are copyrighted material and are not intended to be used as press releases. For reprint requests, please see our Content Usage Policy.




