Adapting CAR T-Cell Therapy to Treat Neuroblastoma
The 2nd article in a 3-part series on recent developments and ongoing research in immunotherapy for childhood cancers.
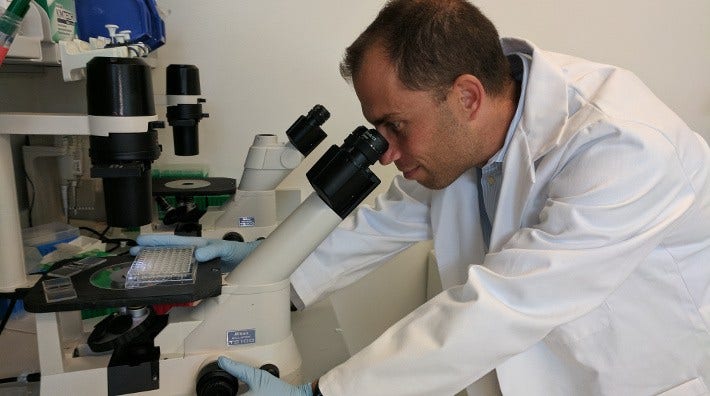
Dr. Andras Heczey, a pediatric oncologist at Texas Children’s Cancer Center examines replicating NKT-cells, part of the process of developing the immunotherapy he is testing for neuroblastoma.
Andras Heczey, MD, spends each day looking for a better way to treat children with neuroblastoma. This solid tumor develops from nerve cells that aren’t in the brain. It occurs most often in infants and young children.
“The 21st century standard of care for neuroblastoma is several cycles of chemotherapy, then even higher doses of chemo with stem cell rescue, followed by radiation, then immunotherapy as maintenance,” he explains. “Still, a large number of patients aren’t cured. In the current age, we should do better. Until we are curing 100% of children using simple, safe approaches, we shouldn’t stop.”
Heczey is a doctor and a researcher at Texas Children’s Cancer Center. He focuses on translational research. That means he takes findings from lab studies and applies them to humans, including in clinical trials.
He started working with his mentor on using immunotherapy to treat neuroblastoma in 2010. Since then, he has evolved and improved upon that original work. “We have an idea of what sort of immunotherapeutic approach may be helpful, and then we test it in preclinical models. If the results are promising, we try to translate what we’ve learned and developed in the lab to a phase 1 clinical trial.”
After 7 years of testing treatment approaches in cells and in mice and showing promising results, Heczey is ready to translate his knowledge into a new cancer immunotherapy to test in children for the first time. With the help of a grant from the American Cancer Society, Heczey is submitting the final approval package to the US Food and Drug Administration (FDA) for a phase 1 clinical trial.
Finding Ways to Make CAR T-Cells Work in Solid Tumors
CAR T-cell treatments are a type of immunotherapy that have seen increasing success in certain blood cancers. For example, recently, a CAR T-cell treatment called Kymriah (tisagenlecleucel) became the first gene therapy to gain approval from the FDA. But the first CAR T-cell studies with solid tumors were disappointing.
To treat a solid tumor with immunotherapy, we have to attack the cancer cells, plus the cells in the tumor that help it grow and the cells that keep the immune system from working.
“I was very excited about CTLO19 making it to market as Kymriah,” Heczey says. “I really wish we could find ways to have similar activity with solid tumors.” But treating them is very different from treating cancer in the blood.
“For successful solid tumor immunotherapy, in addition to finding drugs to attack the cancer cells, we have to find drugs to attack the other components in the tumor. A solid tumor doesn’t just have cancer cells. It has cells that help the cancer grow and cells that try to block the immune system, keeping it from fighting the tumor,” Heczey says.
One way Heczey and his team make progress is by having more than one research project going at a time, allowing him to try several approaches simultaneously. He leads some studies, and he’s a mentor to postdocs and students for others.With several key adaptions, Heczey’s team has learned how to use CAR-T to treat neuroblastoma. To get it to work, they had to:
Find the right kind of white blood cell. Kymriah modifies T-cells with a CAR (chimeric antigen receptor). But T-cells may not work as well in a tumor’s environment.
So, with the help of his mentors Leonid Metelitsa, MD, PhD, and Dr. Malcolm Brenner, MD, PhD, two internationally recognized experts of tumor immunology, Heczey’s team is experimenting with another type of white blood cell—Natural Killer T-cells (NKTs). NKTs can collect in neuroblastoma tumors and attack other white blood cells inside the tumor that help the tumor grow.
Reengineer NKTs. Heczey’s process for developing the treatment for neuroblastoma is similar to the development of CAR T-cells, like Kymriah. A patient has blood drawn. NKTs are separated from that blood and sent to a lab to be genetically modified and increase their numbers, so once the modified NKTs are reinjected into the patient, more cancer cells are destroyed. Heczey’s CARs target the antigen GD2, a molecule called disialoganglioside that’s found on almost all neuroblastoma cells.
When NKTs are equipped with a cancer-targeting molecule called CAR.GD2, they not only continue to attack the white blood cells supporting tumor growth, but they also attack the cancer cells in the tumor.
Make CAR T-cells in solid tumors more effective. With his research team, Heczey learned several ways he can improve how reengineered NKTs duplicate and survive in a patient so they can continue working. They used this knowledge to improve their CAR NKT-cell therapy for neuroblastoma.
Running the Trial
The 2 aims of Heczey’s forthcoming phase 1 clinical trial are to:
- “Describe the safety” of the new drug (CAR.GD2 NKT-cells), which means learn about the side effects it may cause.
- Find the highest tolerated dose of the new drug in children with neuroblastoma.

Dr. Heczey checks the settings of his “molecular copier,” a PCR machine, which copies, or amplifies, DNA segments.
He hopes to start the trial in, or before, the first quarter of 2018. “It depends partly on how many patients are referred to us.” Since the study will be open only at Texas Children’s Cancer Center, patients will have to travel to Houston for the blood collection and treatment.
They plan to gradually increase the dose 4 times, and each dose will be tested in at least 3 patients. That means just going through the incremental dose increases will take time.
“The FDA requested that each time we infuse a patient, we wait 4 weeks before we infuse the next one. If we were lucky enough to have all the patients available and ready, it will take more than a year to finish the study. Of course, patients typically aren’t all immediately ready, and we must be especially careful, since the side effects of CAR NKT-cells are unknown”
The researchers plan to follow the patients who took part in the trial for 15 years.
The Dream That Drives Him
New treatments are first tested in patients who don’t have other treatment options—those whose cancer doesn’t respond to treatment or that keeps coming back. “Once we show that CAR.GD2 NKT-cells work well in patients who’ve had other treatments, we can move toward up-front therapy,” Heczey says.
“My dream, and of course I’m biased, is that we have an approach that is readily available off-the-shelf, so we can get it to the patient more quickly. And, I want all neuroblastoma patients to have to use only one treatment to make their cancer disappear. How quickly can we replace the current chemotherapy, radiation treatment, and immunotherapy approaches? Hopefully in our lifetime. It would be great to see.”




