COVID-19 Pandemic Affects the Cancer Continuum
ACS studies show how COVID-19 is affecting prevention efforts, cancer screening rates, treatment, quality-of-life, and research.
COVID-19 took over the world in 2020 but getting reliable data to understand its effect on cancer takes time—usually 2 to 3 years using traditional population-based data sources like state cancer registries.
Until data started becoming available, researchers had to find innovative ways to gather some facts.
These images and text are a sample of American Cancer Society (ACS) studies published in 2021 based on data found in both traditional and less familiar ways. They show the beginnings of how the COVID-19 pandemic is affecting the continuum of cancer care.
Remembering the Start of the COVID-19 Health Care Takeover
In less than 2 months after the United States identified its first cases of COVID-19, there were more than 100,000 cases and 2,000 deaths.
Everyone attempted to prevent the virus from spreading:
- Most states went into lockdown.
- Local governments advised people to stay home and away from work, school, restaurants, gyms, family—even doctors’ offices and hospitals.
- Many doctors’ offices and hospitals completely shut down non-urgent services and elective procedures, and delayed visits for prevention, screening, treatment, and follow-up care.
Disruptions in health care have affected the full range of cancer care and care for others who may have a higher risk for being hospitalized and dying from coronavirus infection. The pandemic has also increased the risk for people with cancer or with a history of it to have a reduced quality of life due to cancer worry, health anxiety, depression, and inactivity.
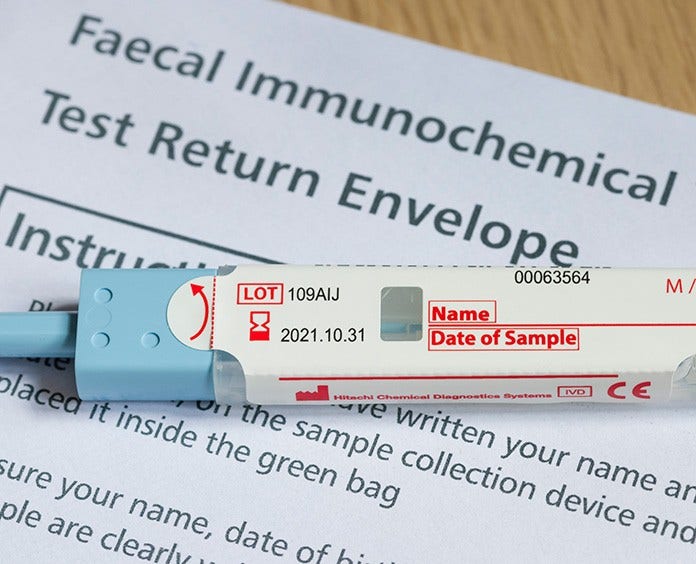
Kudos to Kentucky for Not Letting COVID-19 Curb Lung Cancer Screening
In most states, the COVID-19 pandemic hasn't helped increase the low lung-cancer screening rates of people eligible for a yearly low-dose computed tomography (LDCT).
Surprisingly, though, when ACS researchers compared screening rates between 2019 and 2020, they found 19 states had improved screening rates—with Kentucky having the most improvement.
"Kentucky's screening implementation efforts led to rates more than 2 times the national average and 4 times that of West Virginia and Arkansas, other high lung-cancer burden states.”
—Robert Smith, PhD, study co-author and ACS Senior Vice President, Cancer Screening
- Helpful Resources
- For researchers